
Apollo Gleneagles Hospitals
58 Canal Circular Road,
Kolkata - 700054, WB, India.
Contact : +91 9874167730 / +91 9830363642
Email : pchakrabarti@usa.net

Apollo Gleneagles Hospitals
58 Canal Circular Road,
Kolkata - 700054, WB, India.
Contact : +91 9874167730 / +91 9830363642
Email : pchakrabarti@usa.net

CHRONIC KIDNEY DISEASE OVERVIEW:
Chronic kidney disease (CKD, also called kidney failure) is a condition in which the kidneys lose the ability to remove waste and excess water from the bloodstream. As waste and fluids accumulate, other body systems are affected, potentially leading to complications.
The most common causes of chronic kidney disease are diabetes and high blood pressure. In the early stages of CKD, there are no obvious symptoms. The disease can progress to complete kidney failure, also called end stage renal disease. This occurs when kidney function has worsened to the point that dialysis or kidney transplantation is required to maintain life.
The main goal of treatment is to prevent progression of CKD to complete kidney failure. The best way to do this is to diagnose and control the underlying cause.
NORMAL KIDNEY FUNCTION:
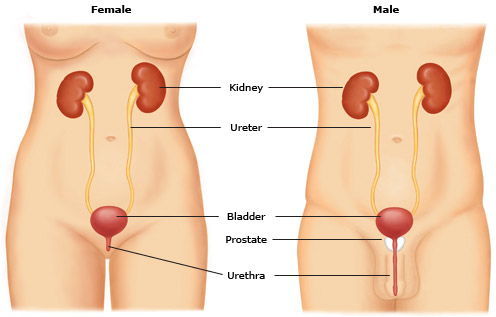
A brief overview of normal kidney function can help in the understanding of chronic kidney disease. The kidneys function to remove wastes and excess water from the blood. These wastes and fluids are combined to form urine. Many vital body functions are dependent upon the proper functioning of the kidneys.
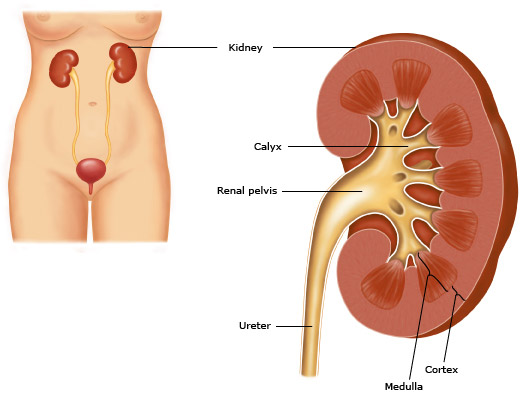
This figure shows the structure of a kidney. The outer portion (the cortex) contains the glomeruli. The tubules are located in the cortex and medulla. The collecting tubules form a large portion of the inner medulla (the papilla). Urine travels from the collecting tubules into the caylces, and then to the renal pelvis, ureter, and bladder.
In order for this filtering process to occur properly, the blood pressure and blood flow to the kidneys must be adequate. If the arteries leading to the kidney are diseased, the filtering process will be affected. The nephrons, including the glomeruli and the tubules, must be healthy, and the path from the nephron to the urethra must not be blocked.
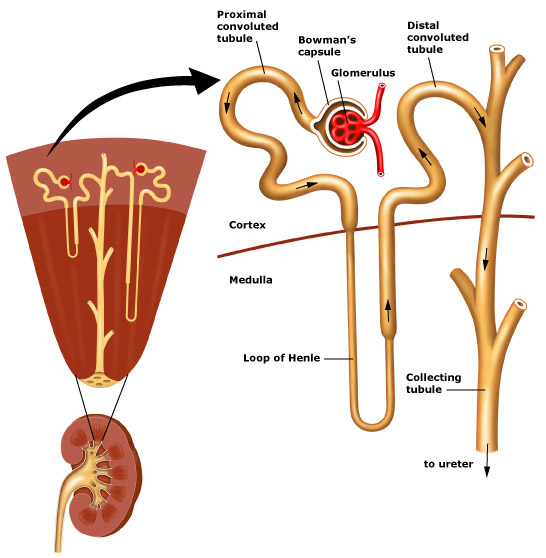
This figure shows the structure of the nephron, which filters waste from the body's blood supply. Each nephron is composed of a glomerulus and a tubule. The glomerulus filters wastes and excess fluids, while the tubules modify the waste to form urine.
When the kidney filters are working properly, the result is a proper balance of fluids and chemicals in the body. If an imbalance occurs, many critical bodily functions can be affected, possibly producing symptoms associated with kidney disease.
This figure shows the structure of the nephron, which filters waste from the body's blood supply. Each nephron is composed of a glomerulus and a tubule. The glomerulus filters wastes and excess fluids, while the tubules modify the waste to form urine.
CHRONIC KIDNEY DISEASE RISK FACTORS:
CHRONIC KIDNEY DISEASE SYMPTOMS:
Most people with chronic kidney disease do not have symptoms until the kidney function is severely impaired. The problem is often discovered when blood or urine tests, done for other reasons, show one or more of the abnormalities discussed above. Even when kidney failure is advanced, most people still make a normal or near-normal amount of urine; this is sometimes confusing. Urine is being formed but it does not contain sufficient amounts of the body's waste products. With advanced kidney disease, you may develop edema (swelling of the feet, ankles, or legs), high blood pressure, blood chemistry (electrolyte) abnormalities, anemia (a decrease in red blood cells, which can cause fatigue and other symptoms), and bone disease. Uremia - People with advanced kidney failure may develop a group of symptoms referred to as uremia. The symptoms of uremia include loss of appetite, nausea, vomiting, swelling around the heart, nerve problems, and changes in mental status, including drowsiness, seizures, or coma.
EVALUATION AND DIAGNOSIS:
A healthcare provider may use several tests to diagnose chronic kidney disease and determine if there is a treatable underlying cause. These include the following: Kidney function tests - The glomerular filtration rate (GFR) gives an approximate measure of the number of functioning nephrons. GFR is used to monitor the severity of kidney impairment. The most common way to estimate the GFR in adults is with several blood tests.
Urine tests - Urine tests can give important information about kidney function. The presence of albumin or protein in the urine (called albuminuria or proteinuria) is a marker of kidney disease. Even small amounts of albumin in the urine, called microalbuminuria, may be an early sign of chronic kidney disease in some people, particularly those with diabetes and high blood pressure.
Imaging studies - Imaging tests (such as CT or ultrasound) may be recommended to determine if there are any obstructions (blockages) of the urinary tract, kidney stones, or other abnormalities.
Renal biopsy - In a renal biopsy, a small piece of kidney tissue is removed and analyzed. The biopsy helps to identify abnormalities in kidney tissue that may be the cause of renal failure.
CHRONIC KIDNEY DISEASE TREATMENT:
The first step in the treatment of chronic kidney disease is to determine the underlying cause. Some causes are reversible, including use of medications that impair kidney function, blockage in the urinary tract, or decreased blood flow to the kidneys. Treatment of reversible causes may prevent CKD from worsening.
Research has shown that management of chronic kidney disease is best done with the assistance of a nephrologist, a doctor who specializes in kidney diseases. Early referral to a nephrologist decreases the chance of developing complications associated with chronic kidney disease.
Hypertension — Hypertension, or high blood pressure, is present in 80 to 85 percent of people with chronic kidney disease. Maintaining good blood pressure control is the most important goal for trying to slow progression of CKD. Taking a medication called angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) reduce blood pressure and levels of protein in the urine, and can slow the progression of chronic kidney disease.
Sometimes, a diuretic (water pill) or other medication is also added. You may be asked to monitor your blood pressure at home to be sure that your blood pressure is well controlled.
Anemia — People with chronic kidney disease are at risk for anemia. This occurs because improperly functioning kidneys produce reduced amounts of a substance called erythropoietin. Anemia can lead to fatigue and other complications.
Selected patients can be treated with drugs that stimulate production of red blood cells. You or a family member can inject these drugs at home. In some cases, iron supplements are also prescribed.
Dietary changes — Changes in your diet may be recommended to control or prevent some of the complications of chronic kidney disease
Protein restriction — Restricting protein in the diet may slow the progression of chronic kidney disease, although it is not clear if the benefits of protein restriction are worth the difficulty of sticking to a low protein diet. Although a reduced protein diet may delay dialysis for several years, the unappetizing nature of the diet is difficult for most people to tolerate. Speak to your healthcare provider about the advantages and disadvantages of a low protein diet.
High potassium — Some people with chronic kidney disease develop a high blood potassium level, which can interfere with normal cell function. This is frequently treated with a diuretic. Measures to prevent high potassium might also be recommended, including a low potassium diet and avoiding medicines that raise potassium levels.
High phosphate — Phosphate is a mineral that helps to keep the bones healthy. Early in the course of chronic kidney disease, the body begins to retain phosphate. As the disease progresses, high blood phosphate levels can develop. This is usually treated with medicines that prevent phosphate (found in foods) from being absorbed in the digestive tract. Dietary phosphate restrictions are also recommended.
High cholesterol and triglycerides — High cholesterol and triglyceride levels are common in people with kidney disease. High triglycerides have been associated with an increased risk of coronary artery disease, which can lead to heart attack.
Treatments to reduce the risk of coronary artery disease are usually recommended, including dietary changes, medications for high triglyceride and cholesterol levels, stopping smoking, and tight blood sugar control in people with diabetes.
Sexual function — Men and women with advanced chronic kidney disease often have difficulties with sexual function and infertility. Over 50 percent of men with end-stage kidney disease have difficulties with erection and decreased sex drive. Women often have disturbances in the menstrual cycle and fertility, usually leading to a stop in menstrual periods. Decreased sex drive may also occur in women.
You should discuss any changes in your sexual function with your healthcare provider because medications or other treatments may be effective.
Pregnancy — The risk that pregnancy will worsen kidney function, or that decreased kidney function will interfere with pregnancy depends upon a number of factors. A woman with mild to moderate chronic kidney disease who is considering becoming pregnant should discuss the possible risks with her nephrologist and obstetrical provider before trying to conceive.
Women with end-stage kidney disease who are on dialysis and who become pregnant are at very high risk for miscarriage, premature delivery, severe hypertension, and preeclampsia. A woman who undergoes successful renal transplantation has a lower risk of these complications. It may be advantageous for a woman to delay becoming pregnant while on hemodialysis if renal transplantation in the near future is likely.
PREPARING FOR DIALYSIS:
Some people with chronic kidney disease progressively worsen over time and will eventually need dialysis. There are two types of dialysis: hemodialysis and peritoneal dialysis. Kidney transplantation is also an option for some people with chronic kidney disease.
An important component of treatment for patients with chronic kidney disease is planning for dialysis in advance. Although kidney transplantation is the treatment of choice in most cases, many people must wait months or years for a kidney to become available. Dialysis will likely be needed, often for an extended period.
Dialysis and kidney transplantation are discussed in detail separately.
Patient information: Chronic kidney disease (The Basics)
What is chronic kidney disease? — Chronic kidney disease is when the kidneys stop working as well as they should. When they are working normally, the kidneys filter the blood and remove waste and excess salt and water.
In people with chronic kidney disease, the kidneys slowly lose the ability to filter the blood. In time, the kidneys can stop working completely. That is why it is so important to keep chronic kidney disease from getting worse.
What are the symptoms of chronic kidney disease? — At first, chronic kidney disease causes no symptoms. As the disease gets worse, it can:
Is there anything I can do to keep my kidneys from getting worse if I have chronic kidney disease? — Yes, you can protect your kidneys by:
What are the treatments for chronic kidney disease? — People in the early stages of chronic kidney disease can take medicines to keep the disease from getting worse. For example, many people with chronic kidney disease should take medicines known as “ACE inhibitors” or “angiotensin receptor blockers.” If your doctor or nurse prescribes these medicines, it is very important that you take them every day as directed. If they cause side effects or cost too much, speak to your doctor or nurse about it. He or she might have solutions to offer.
What happens if my kidneys stop working completely? — If your kidneys stop working completely, you can choose between three different treatments to take over the job of your kidneys. Your choices are described below.
How do I choose between the different treatment options? — You and your doctor will need to work together to find a treatment that's right for you. Kidney transplant surgery is usually the best option for most people. But often there are no kidneys available for transplant.
Ask your doctor to explain all of your options and how they might work for you. Then talk openly with him or her about how you feel about all of the options. You may even decide that you do not want any treatment. That is your choice.
KIDNEY TRANSPLANT
The Benefits of Kidney Transplant
As a kidney transplant recipient, you can expect to feel better physically and emotionally. You will no longer need time-consuming dialysis treatments and can enjoy a more normal diet without fluid restrictions. Relatively quickly, your energy and endurance will increase.
You'll also benefit from the emotional improvements that come with returning to work, travel and recreational activities. Long term, most kidney transplant recipients have a greater life expectancy than can be expected by continuing on dialysis.
While the number of patients nationally with ESRD in need of kidney transplant continues to rise, the number of deceased donor organs available has risen more slowly, creating a long waiting time for those awaiting kidney transplantation. As a result, many people choose to help a family member, loved one or a friend by donating one of their healthy kidneys.
New anti-rejection medications allow ESRD patients to successfully receive kidneys not only from blood relatives, but also from unrelated individuals, such as spouses or friends.
Any potential living donor at our program will receive counseling on the possible risks and complications, and undergo a thorough evaluation to ensure there are no abnormalities that would increase the risk of surgery for either the donor or the recipient.
Laparoscopic donor nephrectomy is a minimally invasive procedure to remove the living donor kidney using operating telescopes. Living donors can expect laparoscopic kidney removal, offering a quicker recovery and less pain from surgery.