
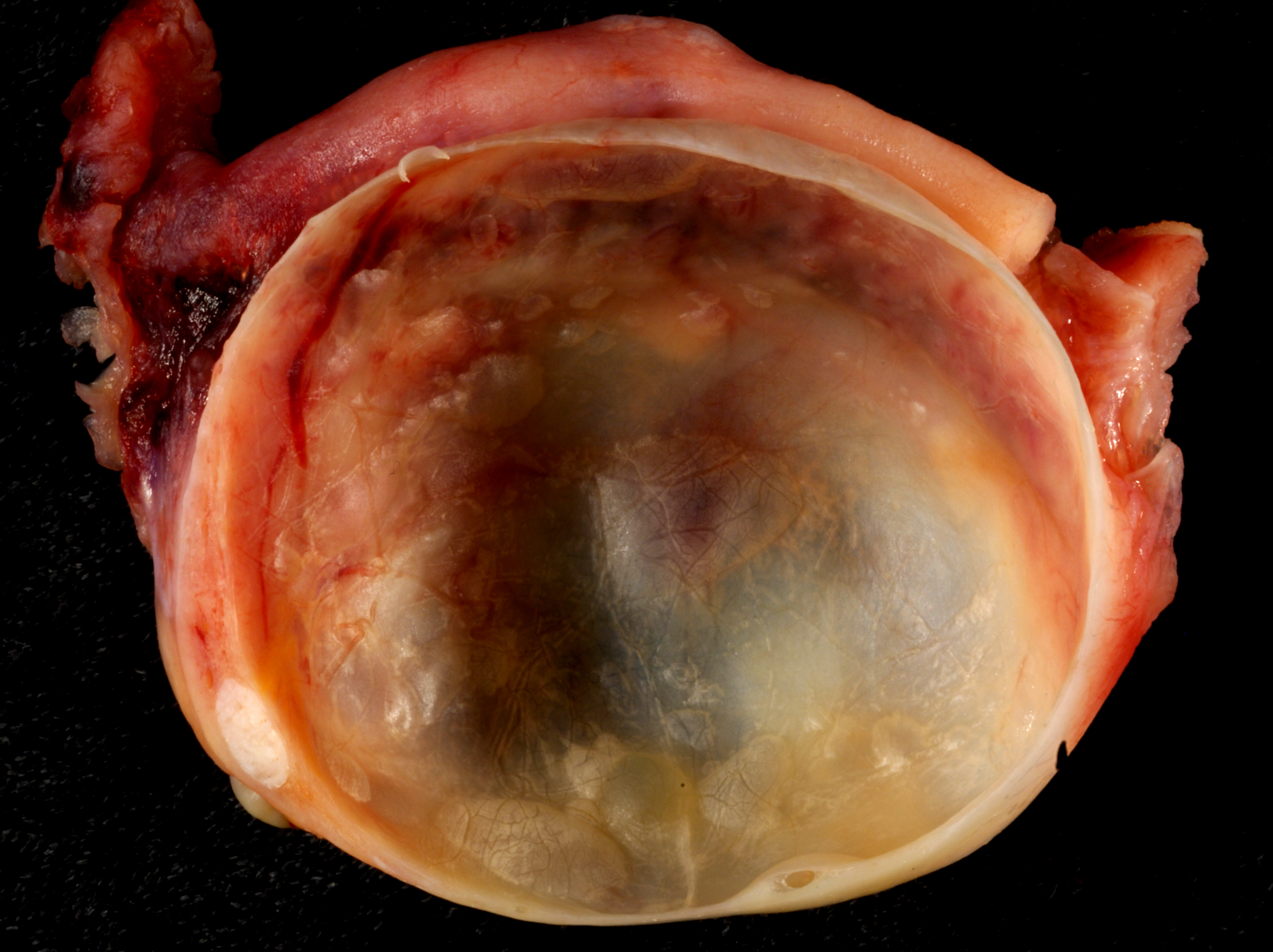
Ovarian cysts
Ovarian cysts are fluid-filled sacs or pockets in an ovary or on its surface. Women have two ovaries - each about the size and shape of an almond - on each side of the uterus. Eggs (ova), which develop and mature in the ovaries, are released in monthly cycles during the childbearing years.
Many women have ovarian cysts at some time. Most ovarian cysts present little or no discomfort and are harmless. The majority disappears without treatment within a few months.
However, ovarian cysts - especially those that have ruptured - can cause serious symptoms. To protect your health, get regular pelvic exams and know the symptoms that can signal a potentially serious problem.
What is a laparoscopic ovarian cystectomy?
An ovarian cystectomy is surgery to remove a cyst from your ovary. Laparoscopic surgery is a minimally invasive surgery technique that only uses a few small incisions in your lower abdomen.
Risk factors
Your risk of developing an ovarian cyst is heightened by:
. Hormonal problems. These include taking the fertility drug clomiphene (Clomid), which is used to cause you to ovulate.
. Pregnancy. Sometimes, the cyst that forms when you ovulate stays on your ovary throughout your pregnancy.
. Endometriosis. This condition causes uterine endometrial cells to grow outside your uterus. Some of the tissue can attach to your ovary and form a growth.
. A severe pelvic infection. If the infection spreads to the ovaries, it can cause cysts.
. A previous ovarian cyst. If you've had one, you're likely to develop more.
Salpingectomy :
Salpingectomy is the surgical removal of one (unilateral) or both (bilateral) fallopian tubes. Fallopian tubes allow eggs to travel from the ovaries to the uterus.
A partial salpingectomy is when you have only part of a fallopian tube removed.
Another procedure, salpingostomy (or neosalpingostomy), is when the surgeon makes an opening in the fallopian tube to remove its contents. The tube itself isn't removed.
Salpingectomy can be done alone or combined with other procedures. These include oophorectomy, hysterectomy, and cesarean section (C-section).
Why is this done ?
Salpingectomy can be used to treat a variety of problems. Your doctor might recommend it if you have:
. an ectopic pregnancy
. a blocked fallopian tube
. a ruptured fallopian tube
. an infection
. fallopian tube cancer
Fallopian tube cancer is rare, but it's more common in women who carry BRCA gene mutations. Fallopian tube lesions occur in up to about half of women with BRCA gene mutations who also have ovarian cancer.
Approaches to salpingectomy
A surgeon may perform a salpingectomy one of two ways. They may make an open incision in the abdomen, in a procedure called a laparotomy.
Or, they may use laparoscopy, which is a minimally invasive approach that involves inserting instruments into small incisions in the lower abdomen.
Surgeons may also perform salpingectomy alongside other procedures. For example, they may do so during cesarean sections in women who have opted for salpingectomy as a method of contraception.
The procedure can vary and involve removing additional organs. Examples of these approaches include:
Partial salpingectomy
This involves removing one fallopian tube. It may be the right approach for an ectopic pregnancy, an infected fallopian tube, or cancer in one tube.
Bilateral salpingectomy
This involves removing both tubes. A surgeon uses this approach when the goal of the procedure is contraception, reducing the risk of ovarian cancer, or treating certain gynecological conditions.
Salpingo-oophorectomy
This approach involves removing one or both ovaries and fallopian tubes. It may help treat ovarian cancer, endometriosis, or ovarian torsion, which is the twisting of an ovary. The surgeon may also choose this approach to ectopic pregnancy.
Myomectomy
Myomectomy is a surgical procedure to remove uterine fibroids - also called leiomyomas (lie-o-my-O-muhs). These common noncancerous growths appear in the uterus. Uterine fibroids usually develop during childbearing years, but they can occur at any age.
The surgeon's goal during myomectomy is to take out symptom-causing fibroids and reconstruct the uterus. Unlike a hysterectomy, which removes your entire uterus, a myomectomy removes only the fibroids and leaves your uterus.
Women who undergo myomectomy report improvement in fibroid symptoms, including decreased heavy menstrual bleeding and pelvic pressure.
Why it's done
Your doctor might recommend myomectomy for fibroids causing symptoms that are troublesome or interfere with your normal activities. If you need surgery, reasons to choose a myomectomy instead of a hysterectomy for uterine fibroids include:
. You plan to bear children
. Your doctor suspects uterine fibroids might be interfering with your fertility
. You want to keep your uterus
Risks
Myomectomy has a low complication rate. Still, the procedure poses a unique set of challenges. Risks of myomectomy include:
. Excessive blood loss. Many women with uterine leiomyomas already have low blood counts (anemia) due to heavy menstrual bleeding, so they're at a higher risk of problems due to blood loss. Your doctor may suggest ways to build up your blood count before surgery.
During myomectomy, surgeons take extra steps to avoid excessive bleeding. These may include blocking flow from the uterine arteries by using tourniquets and clamps and injecting medications around fibroids to cause blood vessels to clamp down. However, most steps don't reduce the risk of needing a transfusion.
In general, studies suggest that there is less blood loss with hysterectomy than myomectomy for similarly sized uteruses.
. Scar tissue. Incisions into the uterus to remove fibroids can lead to adhesions - bands of scar tissue that may develop after surgery. Laparoscopic myomectomy may result in fewer adhesions than abdominal myomectomy (laparotomy).
. Pregnancy or childbirth complications. A myomectomy can increase certain risks during delivery if you become pregnant. If your surgeon had to make a deep incision in your uterine wall, the doctor who manages your subsequent pregnancy may recommend cesarean delivery (C-section) to avoid rupture of the uterus during labor, a very rare complication of pregnancy. Fibroids themselves are also associated with pregnancy complications.
. Rare chance of hysterectomy. Rarely, the surgeon must remove the uterus if bleeding is uncontrollable or other abnormalities are found in addition to fibroids.
. Rare chance of spreading a cancerous tumor. Rarely, a cancerous tumor can be mistaken for a fibroid. Taking out the tumor, especially if it's broken into little pieces (morcellation) to remove through a small incision, can lead to spread of the cancer. The risk of this happening increases after menopause and as women age.
In 2014, the Food and Drug Administration (FDA) cautioned against using a laparoscopic power morcellator for most women undergoing myomectomy. The American College of Obstetricians and Gynecologists (ACOG) recommends you talk to your surgeon about the risks and benefits of morcellation.