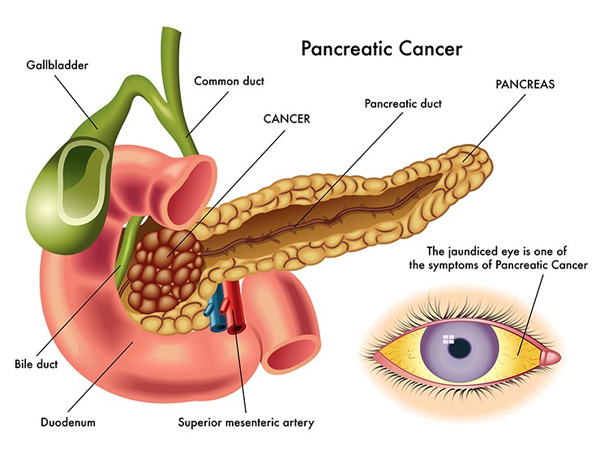
The pancreas is an organ located in the abdomen behind the stomach. It produces both digestive enzymes and insulin.
Pancreatic cancer, in spite of arising as a thirteenth cancer worldwide, is the fourth most common cause of death due to cancer. The incidence and mortality rates of PC have been increasing year by year worldwide.
Most pancreatic tumors are exocrine tumors, including ductal adenocarcinoma, acinar cell carcinoma, cystadenocarcinoma, adenosquamous carcinoma, signet ring cell carcinoma, hepatoid carcinoma, colloid carcinoma, undifferentiated carcinoma, pancreatoblastoma, and pancreatic mucinous cystic neoplasm. And the most common form is ductal adenocarcinoma characterized by moderately to poorly differentiated glandular structures, comprising 80% to 90% of all pancreatic tumors.
Risk Factors:
The possible risk factors for PC include gender, age, smoking, alcohol abuse, obesity, physical activities, diabetes, chronic pancreatitis, vitamin D, genetic alterations, dietary, and reproductive factors.
Diagnosis and Staging:
Early and accurate diagnosis of PC, which often can be challenging, is important because it helps doctors choose the effective and timely treatment option for patients. It is usually based on a combination of imaging techniques such as computer tomography (CT) and endoscopic ultrasonography (EUS), tumor markers such as carbohydrate antigen 19-9 (CA19-9), clinical presentations, and the “gold standard” diagnosis-biopsy.
Clinical Presentation:
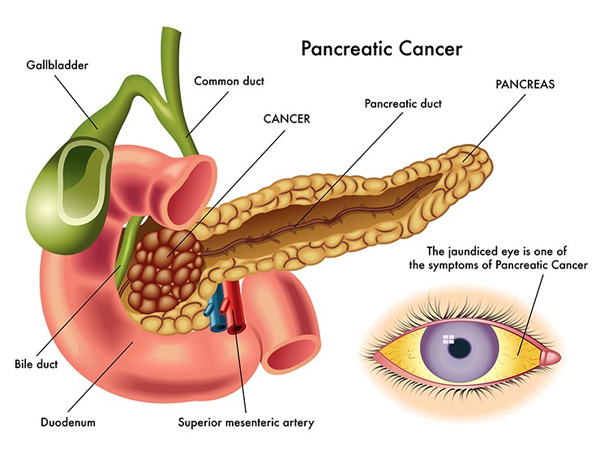
To date, lack of symptoms is the main cause of its late diagnosis and therapy. The appearance of clinical presentations usually indicates an advanced stage and the most frequent presentations are progressive weight loss, anorexia, abdominal pain, and jaundice. These symptoms of PC are nonspecific and varied in different parts of pancreas.
The tumor in the head of the pancreas (75%) produces symptoms such as weight loss, painless jaundice, nausea, and vomiting. The mass of pancreatic head causes blockage of the common bile duct, which results in jaundice, dark urine, light stool color, and itching. Weight loss may be related to malabsorption of nutrients due to PC. Nausea, vomiting, and poor appetite, due to cancer-related gastric outlet (duodenum) obstruction, may also contribute to weight loss.
If cancer is located at the body/tail of the pancreas, patients usually present with abdominal pain that radiates to the sides or the back.
Imaging:
Over the years, imaging techniques, such as transabdominal ultrasound (US), CT, magnetic resonance imaging (MRI), positron emission tomography- (PET-) CT, endoscopic retrograde cholangiopancreatography (ERCP), and EUS, play a vital role in PC detection and staging.
Surgical Resection:
Surgery remains the only possibility for curing of PC, though there are only 20% of patients with operable PC. The selection of an operative procedure for PC is based on factors such as the tumor location, tumor size, and tumor staging.
The classic Whipple procedure (pancreatoduodenectomy), which involves removing the pancreatic head, as well as the curve of the duodenum, the gallbladder, and the common bile duct, is the most common operation for cancers of the head and/or neck of pancreas.
When cancer involves the body and tail, distal/subtotal pancreatectomy is suggested. About 35% of the patients with body/tail PC were observed at the time of surgery, finding that the tumors have spread to surrounding tissues. In such cases, extended resection should be advisable. For patients with locally advanced pancreatic cancer (LAPC), multivisceral resection is technically feasible. Based on recent publications, perioperative mortality (3%) and morbidity (35%) did not differ between two groups of patients who underwent standard resection or multivisceral resection. Although laparoscopy for PC treatment is controversial, laparoscopy in diagnosis and staging of PC is known to be critical, safe, and reliable. Refinements in surgical techniques will reduce perioperative morbidity and improve the outcomes.
Chemotherapy:
For unresectable PC, chemotherapy is being extensively used, such as GEM/erlotinib, FOLFIRINOX,GEM/NAB-paclitaxel,GEM/capecitabine, and capecitabine/oxaliplatin (XELOX). However, PC is characterized by a dense desmoplastic reaction which promotes resistance to chemotherapy
Radiotherapy:
For unresectable PC, there is little evidence to support the efficacy of radiotherapy. However, radiotherapy can be used as a palliative treatment option for those unresectable locally advanced tumors. It can kill cancer cells and keep them from growth and recurrence.
ill defined. Data evaluating the use of adjuvant chemotherapy for CC are limited, and for the most part, combine patients with intrahepatic and extrahepatic CC, gallbladder cancer, and ampullary and pancreatic cancer.