Duodenum & Small Intestine Cancer
Cancer of the small bowel is rare, accounting for 1% of gastro-intestinal malignancies. Adenocarcinomas are the most common of small bowel malignancies, followed by carcinoid tumours, lymphomas, and leiomyosarcomas. Around half of all small bowel adenocarcinomas are located in the duodenum, making this the most favoured site.
Risk Factors for Small Intestine Cancer (Adenocarcinoma):
• Sex: Small intestine cancer occurs slightly more often in men than in women.
• Age: Cancers of the small intestine tend to occur more often in older people. They are most often found in people in their 60s and 70s.
• Race/ethnicity
• Smoking and alcohol use
• Diet: Some research has suggested that diets high in red meat and salted or smoked foods might raise the risk of small intestine cancer.
• Celiac disease
• Colon Cancer: People who have had colon cancer have an increased risk of getting cancer of the small intestine.
• Crohn’s Disease: Crohn’s disease is a condition in which the immune system attacks the gastrointestinal (GI) tract. This disease can affect any part of the GI tract, but it most often affects the lower part of the small intestine. People with this condition have a much higher risk of small intestine cancer (particularly adenocarcinoma).
• Inherited syndromes: People with certain inherited conditions have a higher risk of small intestine cancer (mainly adenocarcinoma).
• Familial adenomatous polyposis (FAP)
• Lynch syndrome (hereditary nonpolyposis colorectal cancer, or HNPCC)
• Peutz-Jeghers syndrome (PJS)
• Cystic fibrosis (CF): People with CF have an increased risk of small intestine cancer
Clinical Presentation
The clinical presentation and diagnosis of SBA is usually delayed. The symptoms are initially rather non-specific.
Symptoms:
• Blood in the stool (feces)
• Dark/black stools
• Diarrhea
• A lump in the abdomen
• Pain or cramps in the abdomen
• Unexplained weight loss
• Episodes of abdominal pain that may be accompanied by severe nausea or vomiting.
Diagnosis
• CT scans have an overall accuracy rate of 47%.
• It should be pointed out that in a context of obscure bleeding after upper and lower endoscopy, a small bowel investigation should systematically be done. New investigation tools, such as CT enteroclysis, MR enteroclysis, capsule endoscopy now allow for an extensive exploration of small bowel and should thus make early diagnosis possible.
Treatment
Localised Cancer
Complete resection (R0) of the primary tumour with loco-regional lymph node resection is mandatory. In the context of posterior invasion, pre-operative treatment should be considered, and resection reconsidered after 2–3 months of chemotherapy.
In the context of unresectable metastases, primary tumour resection is not recommended except in an emergency such as bowel obstruction, perforation or uncontrolled bleeding.
For duodenal tumours, a Whipple resection should be performed for a tumour in the second segment of the duodenum or for an infiltrating tumour in the proximal or distal duodenum.
A duodenal resection alone could be performed for a proximal duodenal tumour or a distal duodenal tumour with no infiltration of adjacent organs.
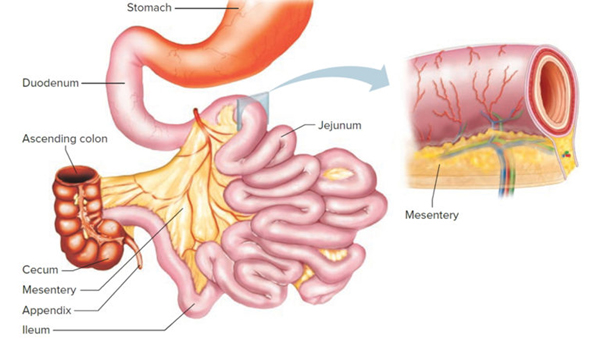
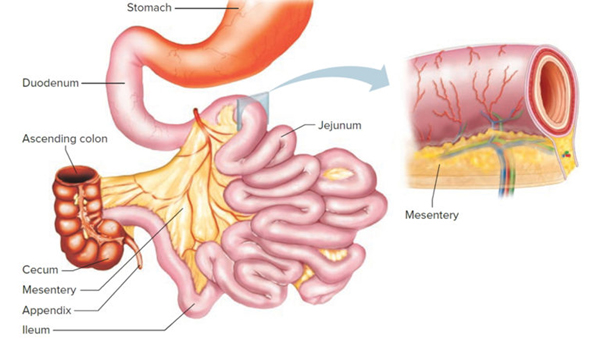
For jejunal and ileal tumours, an R0 resection with lymph node resection and jejuno-jejunal or ileo-ileal anastomosis should be performed.
If the last ileal loop or Bauhin’s valve are involved, an ileocoecal or right hemicolectomy should be performed with ligation of the ileocolic artery so as to allow for lymph node resection.