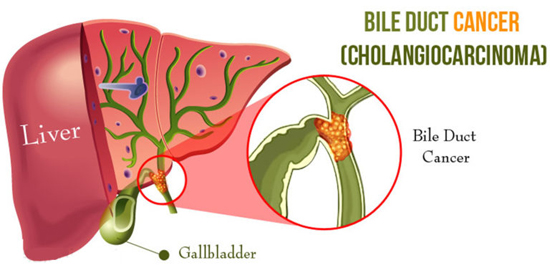
Bile duct neoplasms are rare tumours with overall poor prognosis. The bile duct is a thin tube, about 10 centimetres to 15 centimetres long, that carries a fluid called bile from the liver and gallbladder to the small intestine. Here the bile helps digest the fat in your food. Bile duct cancer can start in any part of the bile duct.
The most common type of bile duct cancers is adenocarcinoma, also called cholangiocarcinona where cancer cells develop in mucus glands (group of cells that produce fluid) that line the inside of the bile duct.
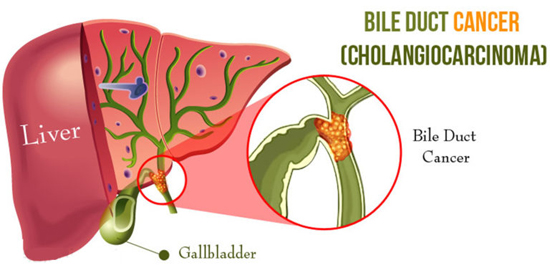
Bile duct cancer is divided into 3 groups based on the cancer’s location:
• Intrahepatic bile duct cancers (within the liver)
• Perihilar bile duct cancers (ducts leaving the liver)
• Distal bile duct cancers (ducts closer to the small intesting.
Common symptoms:
• Jaundice (yellow skin)
• Itchiness all over your body
• Light-coloured stools or dark yellow urine
• Abdomen pain
• Appetite loss or weight loss
• Nausea or vomiting
• Fever
Imaging
Basic imaging methods for hepatobiliary tumours are:
• Ultrasonography,
• Computed Tomography (CT)
• Magnetic Resonance Imaging (MRI)
Further methods include Endosonography, Cholangiography (endoscopic or percutaneous), Positron Emission Tomography (PET), Cholescintigraphy and Angiography
Tumour Markers
Serum tumour markers linked to bile duct carcinomas are:
• carcino-embryogenic antigen (CEA)
• carbohydrate antigen CA 19-9.
The latter has for values above 100 U/mL a sensitivity of 75 % and specifi city of 80 %.
Treatment:
Treatment can be curative (with intent to cure, aiming for long term survival) or palliative (aiming to prolong survival and/or improve life quality and postpone disease symptoms).
The only standard curative option is the complete surgical resection.
Unfortunately, most patients (nearly 90% according to some authors) are not candidates for curative treatment. It is usually for unresectable advanced/metastatic tumour. Some patients are not capable of radical surgery due to their performance status. In these and other cases that sadly form the majority of clinical situations, palliative care is the option.
Preoperative Treatments:
1) BiliaryDrainage: Preoperative biliary drainage has proved to be beneficial in the presence of cholangitis, severe malnutrition, and coagulation abnormalities, and it is absolutely indicated for patients requiring major hepatic resection for curative surgery.
Prolonged preoperative jaundice is associated with increased postoperative morbidity and mortality after hepatic resection due to severe cholestatic liver dysfunction.
2) Portal Vein Embolization: Hilar cholangiocarcinoma usually requires extended hepatectomy (i.e. extended right hepatectomy, and right or left trisegmentectomy), which is related with a rather high rate of perioperative mortality (0% to 19%). This is partly due to the increased rate of postoperative liver failure with major hepatic resection. Portal vein embolization, which was first indicated for hilar cholangiocarcinoma by Makuuchi et al, is now widely accepted as a valuable preoperative measure in anticipation of extensive liver resection with a subsequent small liver remnant volume. Compensatory hypertrophy of the remnant liver parenchyma, usually an increase of 8% to 20% within 2 to 6 wk, is induced in association with atrophy of the future resected liver by selectively occluding the main portal branch to the liver parenchyma to be removed. In general, portal vein embolization can benefit patients requiring a future liver remnant volume of less than 25% to 35% of the original liver volume.
Surgical Management (Resectable Tumours) :
Pancreaticoduodenectomy (Whipple’s PD): Coupled with porta hepatis lymphadenectomy, is the standard treatment of choice for the complete removal of distal bile duct cancer.
Extended hepatectomy for Hilar Cholangiocarcinoma: Based on the mode of tumor extension and the radicality and simplicity of the procedure, extended right- or left hemihepatectomy is regarded as the standard radical operation for hilar cholangiocarcinoma.
Liver Transplantation for Hilar Cholangiocarcinoma: For the treatment of locally advanced hilar cholangiocarcinoma beyond the indication for resection, orthotopic liver transplantation (OLT) may offer the advantage of resection of all structures involved by the tumor, including vessels within the hepatoduodenal ligament, all intraand extrahepatic bile ducts, and whole liver parenchyma.
Prognostic Factors and Markers:
Prognostic factors are:
• Completeness of resection,
• Lymph node involvement and
• Tumour diff erentiation.
These influence the long-term survival of the patient.