Whats is GERD?
Gastroesophageal Reflux Disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus.
Many people experience acid reflux from time to time. GERD is mild acid reflux that occurs at least twice a week, or moderate to severe acid reflux that occurs at least once a week.
Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications or surgery to ease symptoms.
What are the symptoms of GERD?
Common signs and symptoms of GERD include:
• A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
• Chest pain
• Difficulty swallowing
• Regurgitation of food or sour liquid
• Sensation of a lump in your throat
If you have nighttime acid reflux, you might also experience:
• Chronic cough
• Laryngitis
• New or worsening asthma
• Disrupted sleep
When to see a doctor?
Seek immediate medical care if you have chest pain, especially if you also have shortness of breath, or jaw or arm pain. These may be signs and symptoms of a heart attack. Make an appointment with your doctor if you:
• Experience severe or frequent GERD symptoms
• Take over-the-counter medications for heartburn more than twice a week
What causes GERD (Gastro Esophageal Reflux Disease)? What are the risk factors? What are the Complications that could arise?
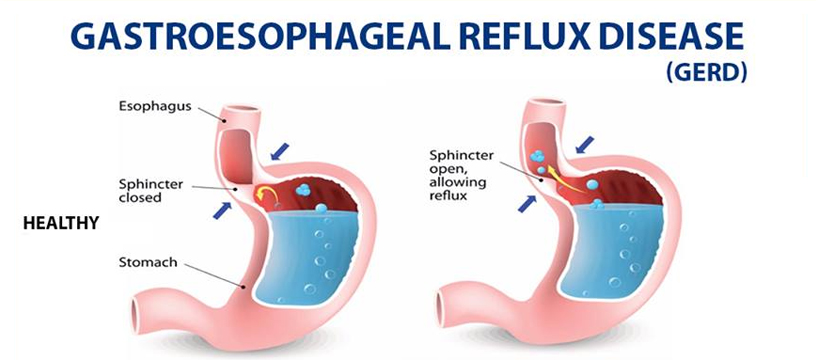
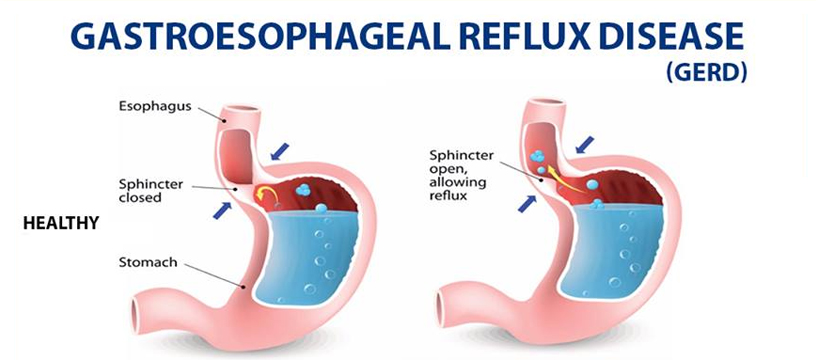
When you swallow, a circular band of muscle around the bottom of your esophagus (lower esophageal sphincter) relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again.
If the sphincter relaxes abnormally or weakens, stomach acid can flow back up into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
Risk Factors
Conditions that can increase your risk of GERD include:
• Obesity
• Bulging of the top of the stomach up into the diaphragm (hiatal hernia)
• Pregnancy
• Connective tissue disorders, such as scleroderma
• Delayed stomach emptying
Factors that can aggravate acid reflux include
• Smoking
• Eating large meals or eating late at night
• Eating certain foods (triggers) such as fatty or fried foods
• Drinking certain beverages, such as alcohol or coffee
• Taking certain medications, such as aspirin
Complications
Over time, chronic inflammation in your esophagus can cause:
• Narrowing of the esophagus (esophageal stricture). Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing.
• An open sore in the esophagus (esophageal ulcer). Stomach acid can wear away tissue in the esophagus, causing an open sore to form. An esophageal ulcer can bleed, cause pain and make swallowing difficult.
• Precancerous changes to the esophagus (Barrett's esophagus). Damage from acid can cause changes in the tissue lining the lower esophagus. These changes are associated with an increased risk of esophageal cancer.
How is (Gastro Esophageal Reflux Disease) treated?
Treatment options include lifestyle modifications, medications, surgery, or a combination of methods.
1) Surgical Treatment of GERD:
The main indication for surgical therapy is failure of medical management when symptoms persist despite appropriate medical therapy. Other indications are development of complications &personal preference.
2) Antireflux Surgery:
Surgery for GERD is known as antireflux surgery and involves a procedure called fundoplication. The goal of this surgery is to reinforce the LES to recreate the barrier that stops reflux from occurring.
Antireflux operations today are most often performed using a minimally invasive surgical technique called Laparoscopic Fundoplication.
The benefit of this type of minimally invasive technique is that it results in less pain, a shorter hospital stay, a faster return to work, smaller scars, and a lower risk of subsequent wound infections and hernias.