An anal fissure is a small cut or tear in the lining of the anus. The crack in the skin causes severe pain and some bright red bleeding during and after bowel movements. At times, the fissure can be deep enough to expose the muscle tissue underneath.
An anal fissure usually isn’t a serious condition. It can affect people of all ages, and it’s often seen in infants and young children since constipation is a common problem in these age groups.
In most cases, the tear heals on its own within four to six weeks. In cases where the fissure persists beyond eight weeks, it’s considered chronic.
Certain treatments can promote healing and help relieve discomfort, including stool softeners and topical pain relievers.
If an anal fissure doesn’t improve with these treatments, you may need surgery. Or your doctor may need to look for other underlying disorders that can cause anal fissures.
What are the symptoms of an Anal Fissure?
An anal fissure may cause one or more of the following symptoms:
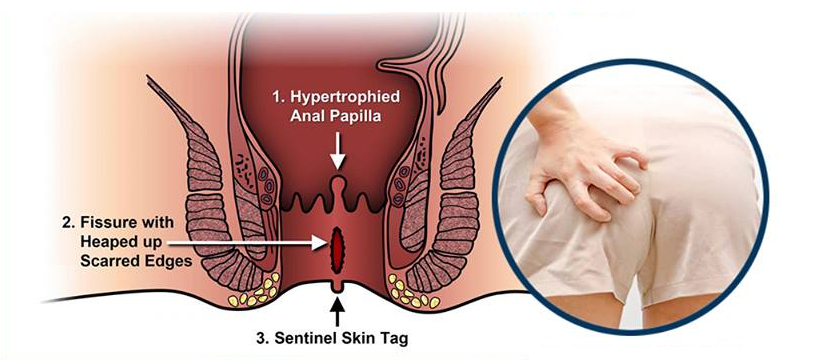
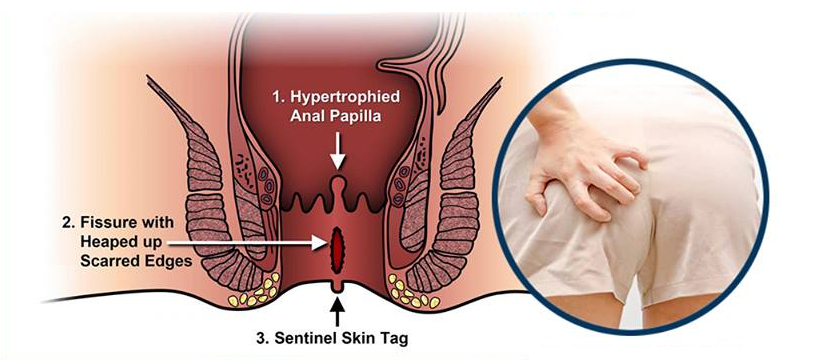
• a visible tear in the skin around your anus
• a skin tag, or small lump of skin, next to the tear
• sharp pain in the anal area during bowel movements
• streaks of blood on stools or on toilet paper after wiping
• burning or itching in the anal area
What causes an Anal Fissure?
An anal fissure most often occurs when passing large or hard stools. Chronic constipation or frequent diarrhea can also tear the skin around your anus.
Other common causes include:
• straining during childbirth or bowel movements
• inflammatory bowel disease (IBD), such as Crohn’s disease
• decreased blood flow to the anorectal area
• overly tight or spastic anal sphincter muscles
In rare cases, an anal fissure may develop due to:
• Anal Cancer
• HIV
• Ttuberculosis
• Syphilis
• Herpes
Who is at Risk for an Anal Fissure?
Anal fissures are common during infancy. Older adults are also prone to anal fissures due to decreased blood flow in the anorectal area. During and after childbirth, women are at risk for anal fissures due to straining during delivery.
People with IBD also have a higher risk for developing anal fissures. The inflammation that occurs in the intestinal lining makes the tissue around the anus more prone to tearing.
People who frequently experience constipation are at an increased risk for anal fissures as well. Straining and passing large, hard stools are the most common causes of anal fissures.
How is an Anal Fissure Treated?
Most anal fissures don’t require extensive treatment.
Depending on your medical record, if permissible, take fibre supplements and eating more fibrous foods, such as raw fruits and vegetables. A sitz bath may relax the anal muscles, relieve irritation, and increase blood flow to the anorectal area. You may apply a nitroglycerin ointment to promote blood flow to the area or a hydrocortisone cream, such as Cortizone 10, to help with inflammation. You may also get some relief by applying topical pain relievers, such as lidocaine, to the anus to ease discomfort
A calcium channel blocker ointment can relax the sphincter muscles and allow the anal fissure to heal.
Another possible treatment is Botox injections into the anal sphincter. The injections will prevent spasms in your anus by temporarily paralyzing the muscle. This allows the anal fissure to heal while preventing new fissures from forming.
If your anal fissure fails to respond to other treatments, your doctor may recommend an anal sphincterotomy. This surgical procedure involves making a small incision in the anal sphincter to relax the muscle. Relaxing the muscle allows the anal fissure to heal.
Not all anal fissures are a sign of low-fiber diets and constipation. Poorly healing fissures or those located in a position other than the posterior and midline portion of your anus may indicate an underlying condition.
If you have any concerns about a fissure that’s not healing despite trying at-home remedies, contact your doctor to see if you need any additional tests.