
Dr. Swapan Kumar De
Senior Most Interventional Cardiologist at
Apollo Multispeciality Hospital Kolkata.
MD, DM (Cardiology)
Peripheral Intervention Specialist in Kolkata, India


Indications for peripheral intervention fall into 2 categories, acute and chronic ischemia. Christopher White, MD (New Orleans, Louisiana, USA), said that the clinical indications for revascularization of acute ischemia include the existence of limb-threatening ischemia and the potential for relief of rest pain. The currently accepted standards for classification of acute ischemia are the SVS/ISCVS criteria, which specify 3 categories: viable, threatened, and irreversible. Treatment options include either surgical thrombectomy or bypass or thrombolytic therapy, with or without balloon angioplasty. Thrombolytic therapy has the advantage of avoiding catheter trauma to the endothelium, or lysis of thrombi distal to the occlusion, but may be associated with a delay in reperfusion of several hours. Absolute contraindications to thrombolysis include active bleeding, recent stroke, and a nonviable target limb.
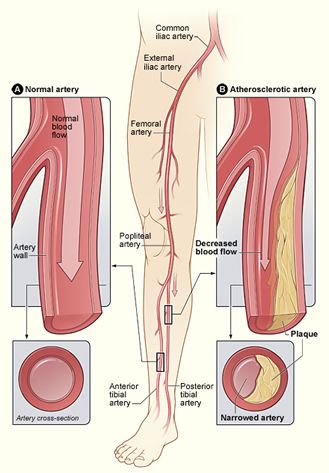
Indications for percutaneous intervention in chronic, lower-extremity ischemia include vascular access, life-style -- limiting claudication, rest pain, nonhealing ulcer, and limb-threatening ischemia. There are 3 lesion subsets for possible intervention, including iliac, femoral-popliteal, and below-knee lesions.
Iliac lesions are associated with very high success rates and low restenosis rates; stents work very well in these lesions. One caveat to remember is the higher-than-usual incidence of associated vessel rupture when the external iliac artery is treated.
Femoral-popliteal lesions have a moderate success rate and a relatively high restenosis rate, but are generally at low risk for procedural complications. The femoral-popliteal vessels require self-expanding stents to prevent external compression and suffer a relatively high restenosis rate, owing to excessive intimal hyperplasia. Caution is necessary when treating these lesions in order to avoid the risk of distal embolization.
Decisions to treat below-knee lesions must be balanced against the increased risk of complications associated with failed attempts, a higher restenosis rate in these smaller vessels, and the common association of diffuse disease in these vessels. Limb viability requires a single, patent vessel, and successful angioplasty of the sole remaining vessel often provides enough circulation to heal a stasis ulcer, independently of the occurrence of restenosis.
The spectrum of intervention ranges from conservative to aggressive. The conservative approach holds that the indications for intervention should be equal to the indications for surgical therapy, that lower-extremity disease is usually not life-threatening, that results are imperfect and restenosis may occur, and that complications are unpredictable. Those who support a more aggressive approach acknowledge the lower risk and lower cost associated with interventional procedures and the fact that restenosis after intervention does not equal a failed bypass surgery.

The potential benefits of intervention -- symptom relief, avoiding surgery, and preserving organ function -- must be balanced against the risk of complications, including atheroemboli, risk of abrupt occlusion, and potential limb loss. The decision of when to intervene is affected by lesion morphology, lesion physiology, and the clinical setting. Patients with claudication tend to have better outcomes than those with limbs at risk. Discrete lesions are associated with better outcomes than diffuse lesions, and stenoses have more favorable outcomes than occlusions.
Peripheral Artery Stenting
Hardening of the arteries, also known as atherosclerosis, can cause the build up of plaque. In hardening of the arteries, plaque builds up in the walls of your arteries as you age. Cholesterol, calcium, and fibrous tissue make up the plaque. As more plaque builds up, your arteries can narrow and stiffen. Eventually, enough plaque may build up to reduce blood flow through your arteries, or cause blood clots or pieces of the plaque to break away and block the arteries in the brain beyond the plaque.
Carotid Artery Stenting
Carotid artery stenting is a procedure in which your physician inserts a slender, metal-mesh tube, called a stent, which expands inside your carotid artery to increase blood flow in areas blocked by plaque.
Renal Artery Stenting
Renal artery stenting is a procedure in which your physician inserts a slender, metal-mesh tube, called a stent, which expands inside your renal artery to increase blood flow in areas blocked by plaque.
Inferior Vena Cava (IVC) Filter Placement
The IVC is a major blood vessel that returns blood from the lower body to the heart. An IVC filter is a small piece of metal that can be put into the inferior vena cava to prevent blood clots in the legs from going up to the lungs.
A blood clot in the leg is called a deep vein thrombosis (DVT). If the clot goes to the lung, it's called a pulmonary embolus (PE). A large PE can be lethal.
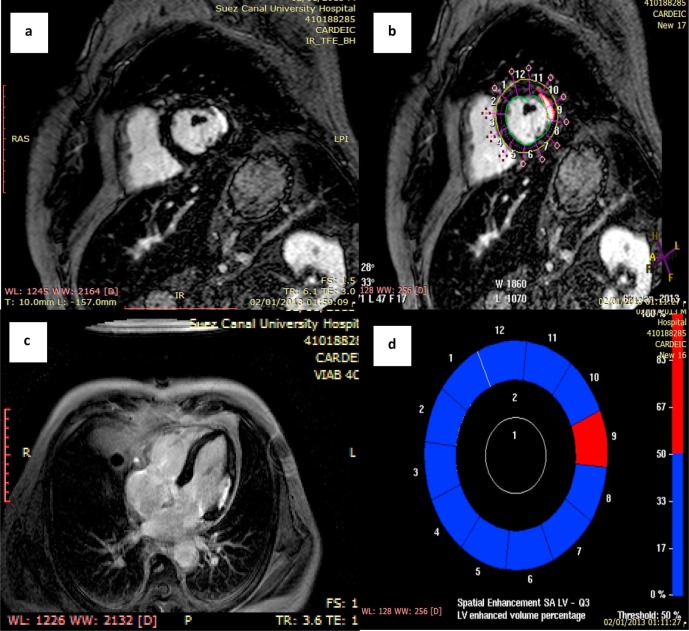
About Cardiologists : Cardiologists treat people with diseases or conditions of the heart and people who want to learn the risk factors for heart disease. A primary care doctor or family practice doctor can work with a cardiology specialist to diagnose, treat, and manage heart conditions and help people make heart-healthy lifestyle choices. Patients who are at risk for heart disease or have a history of heart symptoms may see a clinical cardiologist regularly. People with ongoing heart conditions, pacemakers, or frequent heart trouble are likely to see a cardiologist with a subspecialty.