Treatment : |
| |
| Shoulder Surgery : |
| |
Your shoulder is the most flexible joint in your body. It allows you to place and rotate your arm in many positions in front, above, to the side, and behind your body. This flexibility also makes your shoulder susceptible to instability and injury.
Depending on the nature of the problem, nonsurgical methods of treatment often are recommended before surgery. However, in some instances, delaying the surgical repair of a shoulder can increase the likelihood that the problem will be more difficult to treat later. Early, correct diagnosis and treatment of shoulder problems can make a significant difference in the long run.
 Bursitis or Tendinitis Bursitis or Tendinitis
Bursitis or tendinitis can occur with overuse from repetitive activities, such as swimming, painting, or weight lifting. These activities cause rubbing or squeezing (impingement) of the rotator cuff under the acromion and in the acromioclavicular joint. Initially, these problems are treated by modifying the activity which causes the symptoms of pain and with arehabilitation program for the shoulder.
Impingement and Partial Rotator Cuff Tears
 Partial thickness rotator cuff tears can be associated with chronic inflammation and the development of spurs on the underside of the acromion or the acromioclavicular joint. Partial thickness rotator cuff tears can be associated with chronic inflammation and the development of spurs on the underside of the acromion or the acromioclavicular joint.
The conservative nonsurgical treatment is modification of activity, light exercise, and, occasionally, a cortisone injection. Nonsurgical treatment is successful in a majority of cases. If it is not successful, surgery often is needed to remove the spurs on the underside of the acromion and torepair the rotator cuff.
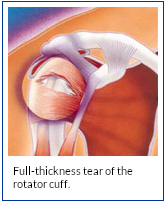
Full-Thickness Rotator Cuff Tears
Full-thickness rotator cuff tears are most often the result of impingement, partial thickness rotator cuff tears, heavy lifting, or falls. Nonsurgical treatment with modification of activity is successful in a majority of cases.
If pain continues, surgery may be needed to repair full- thickness rotator cuff tears. Arthroscopic techniques allow shaving of spurs, evaluation of the rotator cuff, and repair of some tears.
Both techniques require extensive rehabilitation to restore the function of the shoulder. |
| |
Knee Surgery :
If your knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down.
If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities.
Knee replacement surgery was first performed in 1968. Since then, improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacements are one of the most successful procedures in all of medicine. According to the Agency for Healthcare Research and Quality, more than 600,000 knee replacements are performed each year in the United States.
Whether you have just begun exploring treatment options or have already decided to have total knee replacement surgery, this article will help you understand more about this valuable procedure.
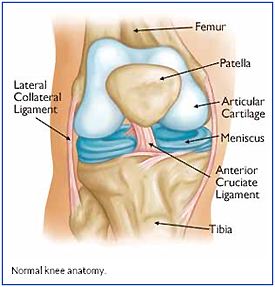 Anatomy Anatomy
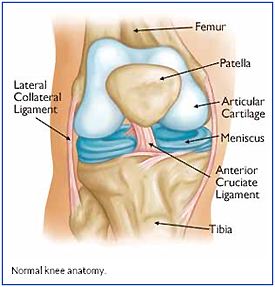
The knee is the largest joint in the body and having healthy knees is required to perform most everyday activities.
The knee is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones where they touch are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily.
The menisci are located between the femur and tibia. These C-shaped wedges act as "shock absorbers" that cushion the joint.
Large ligaments hold the femur and tibia together and provide stability. The long thigh muscles give the knee strength.
All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.
Cause
The most common cause of chronic knee pain and disability is arthritis. Although there are many types of arthritis, most knee pain is caused by just three types: osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
- Osteoarthritis. This is an age-related "wear and tear" type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness.
- Rheumatoid arthritis. This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed "inflammatory arthritis."
- Post-traumatic arthritis. This can follow a serious knee injury. Fractures of the bones surrounding the knee or tears of the knee ligaments may damage the articular cartilage over time, causing knee pain and limiting knee function.
|
| |
| |
Ankle Surgery :
A broken ankle is also known as an ankle "fracture." This means that one or more of the bones that make up the ankle joint are broken.
A fractured ankle can range from a simple break in one bone, which may not stop you from walking, to several fractures, which forces your ankle out of place and may require that you not put weight on it for a few months.
Simply put, the more bones that are broken, the more unstable the ankle becomes. There may be ligaments damaged as well. The ligaments of the ankle hold the ankle bones and joint in position.
Broken ankles affect people of all ages. During the past 30 to 40 years, doctors have noted an increase in the number and severity of broken ankles, due in part to an active, older population of "baby boomers."
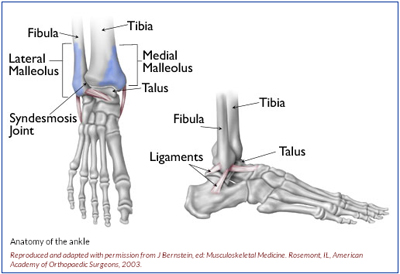 Anatomy Anatomy
Three bones make up the ankle joint:
- Tibia - shinbone
- Fibula - smaller bone of the lower leg
- Talus - a small bone that sits between the heel bone (calcaneus) and the tibia and fibula
The tibia and fibula have specific parts that make up the ankle:
- Medial malleolus - inside part of the tibia
- Posterior malleolus - back part of the tibia
- Lateral malleolus - end of the fibula
Doctors classify ankle fractures according to the area of bone that is broken. For example, a fracture at the end of the fibula is called a lateral malleolus fracture, or if both the tibia and fibula are broken, it is called a bimalleolar fracture.
Two joints are involved in ankle fractures:
- Ankle joint - where the tibia, fibula, and talus meet
- Syndesmosis joint - the joint between the tibia and fibula, which is held together by ligaments
Multiple ligaments help make the ankle joint stable.
Symptoms
Because a severe ankle sprain can feel the same as a broken ankle, every ankle injury should be evaluated by a physician.
Common symptoms for a broken ankle include:
- Immediate and severe pain
- Swelling
- Bruising
- Tender to touch
- Cannot put any weight on the injured foot
- Deformity ("out of place"), particularly if the ankle joint is dislocated as well
|
| |
| |
Elbow Surgery :
Arthroscopy is a procedure that orthopaedic surgeons use to inspect, diagnose, and repair problems inside a joint.
The word arthroscopy comes from two Greek words, "arthro" (joint) and "skopein" (to look). The term literally means "to look within the joint." During elbow arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your elbow joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.
Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for open surgery. This results in less pain for patients, less joint stiffness, and often shortens the time it takes to recover and return to favorite activities.
Elbow arthroscopy has been performed since the 1980s. It has made diagnosis, treatment, and recovery from surgery easier and faster than was once thought possible. Improvements to elbow arthroscopy occur every year as new instruments and techniques are developed. |
| |
| Anatomy |
| |
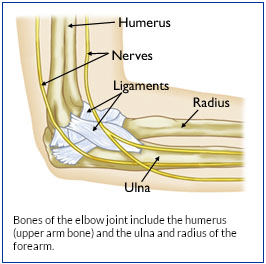 The elbow is a complex joint formed by the joining of three bones: The elbow is a complex joint formed by the joining of three bones:
- The humerus (upper arm bone)
- The ulna (forearm bone on the pinky finger side)
- The radius (forearm bone on the thumb side)
The surfaces of the bones where they meet to form the elbow joint are covered with articular cartilage, a smooth substance that protects the bones and acts as a natural cushion to absorb forces across the joint. A thin, smooth tissue called synovial membrane covers all remaining surfaces inside the elbow joint. In a healthy elbow, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction as you bend and rotate your arm.
On the inner and outer sides of the elbow, thicker ligaments (collateral ligaments) hold the elbow joint together and prevent dislocation.
The elbow joint is surrounded by muscles on the front and back sides. In addition, the three major nerves that cross the elbow joint are located close to the joint surfaces and capsule and must be protected during arthroscopic surgery.
The elbow joint allows two basic movements: bending and straightening (flexion and extension) and forearm rotation (pronation — palm down, and supination — palm up).
Normal bending and straightening motion occurs at the joining of the humerus and ulna bones. Forearm rotation occurs at the joining of the ulna and radius and is also influenced by muscles and ligaments further down the forearm and at the wrist joint. |
|
| |
Hip Surgery :
| A hip fracture is a break in the upper quarter of the femur (thigh) bone. The extent of the break depends on the forces that are involved. The type of surgery used to treat a hip fracture is primarily based on the bones and soft tissues affected or on the level of the fracture. |
| |
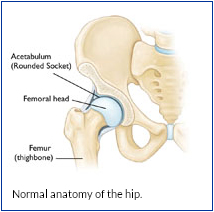
| Anatomy |
| |
The "hip" is a ball-and-socket joint. It allows the upper leg to bend and rotate at the pelvis. An injury to the socket, or acetabulum, itself is not considered a "hip fracture." Management of fractures to the socket is a completely different consideration.
Causes :
 Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting. Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting.
Symptoms :
The patient with a hip fracture will have pain over the outer upper thigh or in the groin. There will be significant discomfort with any attempt to flex or rotate the hip.
If the bone has been weakened by disease (such as a stress injury or cancer), the patient may notice aching in the groin or thigh area for a period of time before the break. If the bone is completely broken, the leg may appear to be shorter than the noninjured leg. The patient will often hold the injured leg in a still position with the foot and knee turned outward (external rotation).
Treatment :
Surgical Treatment
Anesthesia for surgery could be either general anesthesia with a breathing tube or spinal anesthesia. In very rare circumstances, where only a few screws are planned for fixation, local anesthesia with heavy sedation can be considered. All patients will receive antibiotics during surgery and for the 24-hours afterward.
Appropriate blood tests, chest X-rays, electrocardiograms, and urine samples will be obtained before surgery. Many elderly patients may have undiagnosed urinary tract infections that could lead to an infection of the hip after surgery.
The surgeon's decision as to how to best fix a fracture will be based on the area of the hip that is broken and the surgeon's familiarity with the different systems that are available to manage these injuries. |
|
|

 Anatomy
Anatomy 








 Bursitis or Tendinitis
Bursitis or Tendinitis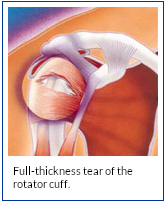 Partial thickness rotator cuff tears can be associated with chronic inflammation and the development of spurs on the underside of the acromion or the acromioclavicular joint.
Partial thickness rotator cuff tears can be associated with chronic inflammation and the development of spurs on the underside of the acromion or the acromioclavicular joint.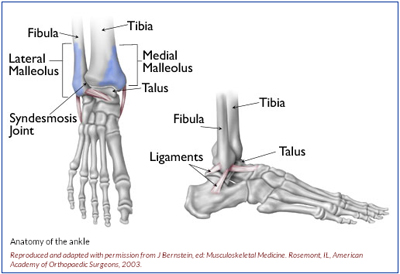 Anatomy
Anatomy 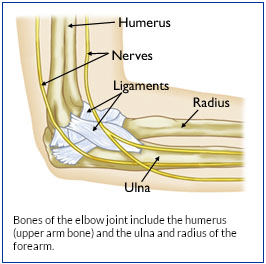 The elbow is a complex joint formed by the joining of three bones:
The elbow is a complex joint formed by the joining of three bones: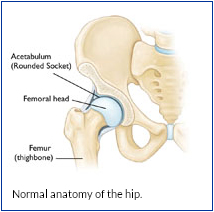 Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting.
Hip fractures most commonly occur from a fall or from a direct blow to the side of the hip. Some medical conditions such as osteoporosis, cancer, or stress injuries can weaken the bone and make the hip more susceptible to breaking. In severe cases, it is possible for the hip to break with the patient merely standing on the leg and twisting.