
Dr. Amitabha Das
MBBS (Hons), MS (General Surgery, Gold medalist), MCh (Neurosurgery, AIIMS

MBBS (Hons), MS (General Surgery, Gold medalist), MCh (Neurosurgery, AIIMS
Minimally Invasive Spine Surgery
Spine surgery is traditionally done as "open surgery." This means that the area being operated on is opened with a long incision to allow the surgeon to view and access the anatomy. In recent years, however, technological advances have allowed more back and neck conditions to be treated with a minimally invasive surgical technique.
Because minimally invasive spine surgery (MISS), does not involve a long incision, it avoids significant damage to the muscles surrounding the spine. Typically, this results in less pain after surgery and a faster recovery.
The indications for minimally invasive spine surgery are the same as those for traditional open surgery. Spine surgery is usually recommended only when a period of nonsurgical treatment — such as medications and physical therapy — has not relieved the painful symptoms caused by your back problem. In addition, surgery is only considered if your doctor can pinpoint the exact source of your pain, such as a herniated disk or spinal stenosis.
 There are numerous minimally invasive techniques. The common thread between all of them is that they use smaller incisions and cause less muscle damage. Minimally invasive techniques can be used for common procedures like lumbar decompression and spinal fusion. Decompression relieves pressure on spinal nerves by removing portions of bone or a herniated disk. Spinal fusion corrects problems with the small bones of the spine (vertebrae). The basic idea is to fuse together the painful vertebrae so that they heal into a single solid bone. This article focuses on decompression and spinal fusion with a minimally invasive technique.
There are numerous minimally invasive techniques. The common thread between all of them is that they use smaller incisions and cause less muscle damage. Minimally invasive techniques can be used for common procedures like lumbar decompression and spinal fusion. Decompression relieves pressure on spinal nerves by removing portions of bone or a herniated disk. Spinal fusion corrects problems with the small bones of the spine (vertebrae). The basic idea is to fuse together the painful vertebrae so that they heal into a single solid bone. This article focuses on decompression and spinal fusion with a minimally invasive technique.
For a complete overview of spinal fusion including approaches, bone grafting, complications, and rehabilitation: Spinal Fusion.
Description
Minimally invasive spine surgery (MISS) is sometimes called less invasive spine surgery. In these procedures, doctors use specialized instruments to access the spine through small incisions.
In a traditional open surgery, the doctor makes an incision that is 5 to 6 inches long, then moves the muscles to the side in order to see the spine. With the muscles pulled to the side, the surgeon can access the spine to remove diseased and damaged bone or intervertebral disks. The surgeon can also easily see to place screws, cages, and any bone graft materials necessary to stabilize the spinal bones and promote healing.
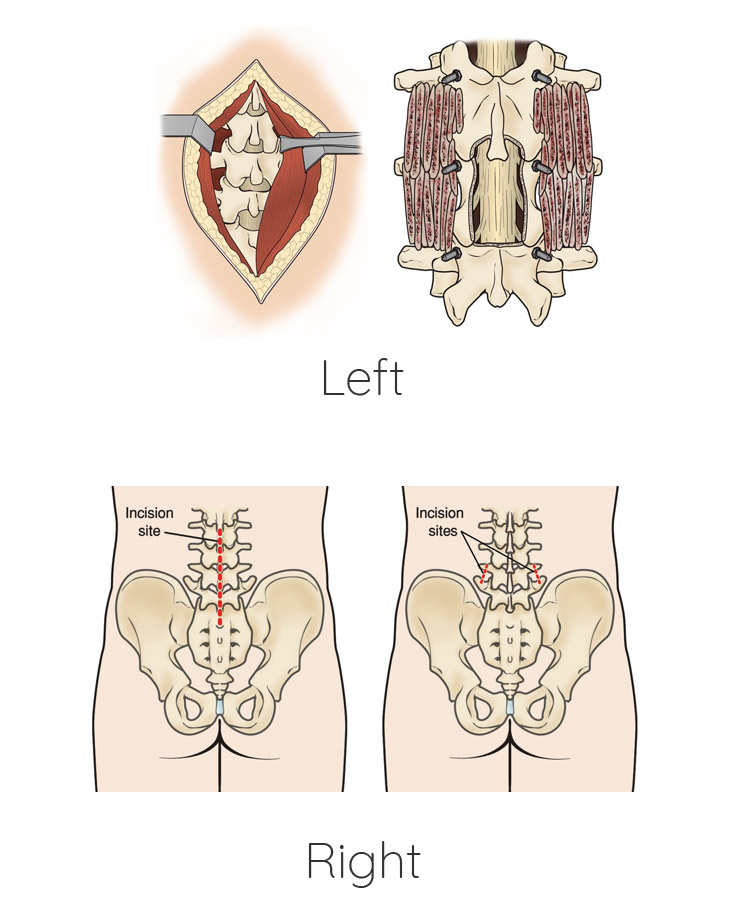 (Left) In traditional open surgery, muscles surrounding the spine are pulled back to reveal the bones. (Right) After removing portions of the bone (a decompression procedure called laminectomy), bone graft material and screws are placed along the sides of the vertebrae.
(Left) In traditional open surgery, muscles surrounding the spine are pulled back to reveal the bones. (Right) After removing portions of the bone (a decompression procedure called laminectomy), bone graft material and screws are placed along the sides of the vertebrae.
One of the major drawbacks of open surgery is that the pulling or "retraction" of the muscle can damage both the muscle and the surrounding soft tissue. Although the goal of muscle retraction is to help the surgeon see the problem area, it typically affects more anatomy than the surgeon requires. As a result, there is greater potential for muscle injury, and patients may have pain after surgery that is different from the back pain felt before surgery. This can lead to a lengthier recovery period. The larger incision and damage to soft tissues may also increase both blood loss and the risk for infection.
Minimally invasive spine surgery was developed to treat spine problems with less injury to the muscles and other normal structures in the spine. It also helps the surgeon to see only the location where the problem exists in the spine. Other advantages of MISS include smaller incisions, less bleeding, and shorter stays in the hospital.
(Left) The incision site in the lower back that is used for some traditional open spine surgeries. (Right)The minimally invasive incisions typically used for a lumbar spinal fusion. Both the decompression and the placing of screws and rods are accomplished through these small incisions.
Conditions Treated Using MIS Procedures
• Degenerative disc disease
• Herniated disc
• Lumbar spinal stenosis
• Spinal deformities such as scoliosis
• Spinal infections
• Spinal instability
• Vertebral compression fractures
• Spinal Tumors
 3
3
Complications
As with any operation, there are potential risks associated with MISS. The complications of MISS are similar to those of open spinal fusion surgeries; however, some studies show a reduced infection rate for MISS. Before your surgery, your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications. The potential complications of MISS include:
A) Infection
Antibiotics are given to the patient before, during, and often after surgery to lessen the risk of infections.
B) Bleeding
A certain amount of bleeding is expected, but this is not typically significant.
C) Pain at Graft Site
A small percentage of patients will experience persistent pain at the bone graft site.
D) Recurring Symptoms
Some patients may experience a recurrence of their original symptoms.
E) Pseudarthrosis
This is a condition in which there is not enough bone formation and a spinal fusion does not completely heal. If this occurs, a second surgery may be needed in order to obtain a solid fusion. Patients who smoke are more likely to develop a pseudarthrosis.
F) Nerve Damage
It is possible that the nerves or blood vessels may be injured during these operations. These complications are very rare.
G) Blood Clots
Formation of blood clots in the legs is another uncommon complication after surgery. They pose a significant danger if they break off and travel to the lungs.
 4
4
How Minimally Invasive Spine Surgery Works
Because the spinal nerves, vertebrae and discs are located deep inside the body, any approach to gain access to the spinal area requires moving the muscle tissue out of the way. In general, this is facilitated by utilizing a small incision (s) and guiding instruments and/or microscopic video cameras through these incisions. Contrary to popular belief, lasers are very rarely used in MIS surgeries.
A number of methods can be used to minimize trauma during MIS surgery. Some of the more common techniques include:
A) Performing the surgery using a tubular retractor:
This technique involves progressive dilation of the soft tissues, as opposed to cutting directly through the muscles. By using tubes to keep the muscles out of the way, the surgeon can work through the incision without having to expose the area widely. Sometimes, the surgeon will also utilize an endoscopic or microscope focused down the tube to assist with performing the surgery through a minimal access strategy. Once the procedure is complete, the tubular retractor can be removed, allowing the dilated tissues to come back together. Depending on the extent and type of surgery necessary, incisions can often be small.
B) Percutaneous placement of screws and rods:
Depending on the condition of the patient, it may be necessary to place instrumentation, such as rods and screws, to stabilize the spine or to immobilize the spine to facilitate fusion of the spinal bones. Traditional approaches for placement of screws requires extensive removal of muscle and other tissues from the surface of the spine.
However, percutaneous (which means “through the skin”) placement typically involves inserting rods and screws through relatively small skin incisions without cutting or dissecting the underlying muscle. With the aid of X-ray images, guidewires are placed through the skin and into the spinal vertebrae along the desired paths for the screws. Then, screws are placed over the guidewires and follow the path of the wires. These screws have temporary extenders that extend outside of the skin and subsequently removed after helping to guide passage of rods to connect and secure the screws.
C) Direct lateral access routes:
In some cases — especially those involving the lumbar spine — approaching the spine from the side of the body results in reduced pain, due to the limited amount of muscle tissue blocking the way. This approach is typically performed with the patient on his or her side. Then, a tubular retractor docks on the side of the spine to enable access to the spine’s discs and bones.
D) Thoracscopic access route:
Depending on the patient's condition, it may be necessary to access the front portions of the thoracic spine, located in the chest and surrounded by the heart and lungs. Traditional access approaches often involve opening the chest through large incisions that may also require removal of one or more ribs. However, thoracscopic access relies on multiple small incisions through which working ports and cameras can be inserted to facilitate surgery.
