Brain Tumors
Types of Brain Tumors -
A brain tumor is an abnormal mass of tissue in which cells grow and multiply uncontrollably, seemingly unchecked by the mechanisms that control normal cells. More than 150 different brain tumors have been documented, but to simplify matters, the two main brain tumor groups are primary and metastatic.
Primary brain tumors include tumors which originate from the tissues of the brain, or the brain’s immediate surroundings. Primary tumors are categorized as glial or non-glial and benign or malignant.
Metastatic brain tumors include tumors which arise elsewhere in the body (such as the breast or lungs) and migrate to the brain, usually through the bloodstream. Metastatic tumors are considered cancer, and are malignant.
Metastatic tumors to the brain affect nearly one in four patients with cancer, or an estimated 150,000 people a year. As many as 40 percent of people with lung cancer will develop metastatic brain tumors. In the past, the outcome for patients with these tumors was very poor, with typical survival rates just several weeks. More sophisticated diagnostic tools, and innovative surgical and radiation approaches can now lead to longer survival and a better quality of life, measured in months to years.
Brain Tumor in an Eloquent Area – Awake Surgery -
Left - sided Low grade Astrocytoma in a computer software engineer with epilepsy and calculation difficulty. Complete resection. Post operative MRI scans and Interview. After 10 years he is seizure free with no recurrence of tumor.
Incidence in Adults -
It is estimated that in 2005, there were a total of 18,500 new cases of brain and other nervous system tumors diagnosed - 10,620 males and 7,880 females. The estimated number of deaths was 12,760, of which 7,280 were males and 5,480 were females.
From 1998-2002, the median age at diagnosis for cancer of the brain and central nervous system was age 55.
Types of benign Brain Tumors -
1) Chordomas are benign, slowly growing tumors that are most prevalent in people ages 50 to 60. Their most common locations are the base of the skull and the lower portion of the spine. Although these tumors are benign, they may invade the adjacent bone and put pressure on nearby neural tissue. These are rare tumors, contributing to only 0.2 percent of all primary brain tumors.
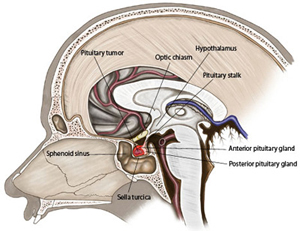
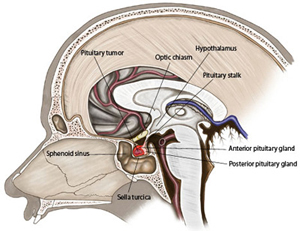
2) Craniopharyngiomas are typically benign, but are difficult tumors to remove because of their location near critical structures deep in the brain. These tumors usually arise from a portion of the pituitary gland (the structure that regulates many hormones in the body), so nearly all patients will require some hormone replacement therapy.
3) Gangliocytomas, gangliomas, and anaplastic gangliogliomas are rare tumors that include neoplastic nerve cells that are relatively well differentiated, occurring primarily in young adults.
4) Glomus jugulare tumors are most frequently benign, and are typically located just under the skull base, at the top of the jugular vein. Glomus jugulare tumors are the most common form of glomus tumor. However, glomus tumors in general contribute to only 0.6 percent of neoplasms of the head and neck.
5) Meningiomas are the most common benign intracranial tumors comprising 10 to 15 percent of all brain neoplasms, although a very small percentage are malignant. These tumors originate from the meninges, the membrane-like structures that surround the brain and spinal cord.
6) Pineocytomas are generally benign lesions that arise from the pineal cells, occurring predominantly in adults. They are most often well-defined, noninvasive, homogeneous, and slow growing.
7) Pituitary Adenomas are the most common intracranial tumor after gliomas, meningiomas and schwannomas. The large majority of pituitary adenomas are benign and fairly slow growing. Even malignant pituitary tumors rarely spread to other parts of the body. Adenomas are by far the most common disease affecting the pituitary. They more commonly affect people in their 30s or 40s, although they are diagnosed in children as well. Most of these tumors can be successfully treated.
8) Schwannomas are common benign brain tumors in adults. They arise along nerves, comprised of cells that normally provide the "electrical insulation" for the nerve cells. Schwannomas often displace the remainder of the normal nerve instead of invading it. Acoustic neuromas are the most common schwannoma, arising from the eighth cranial nerve, or vestibular-cochlear nerve, which travels from the brain to the ear. Although these tumors are benign, they can cause serious complications and even death if they grow and exert pressure on nerves and eventually on the brain. Other locations include the spine, and, more rarely, along nerves that go to the limbs.
Types of malignant Brain Tumors -
1) Gliomas are the most prevalent type of adult brain tumor, accounting for 78 percent of malignant brain tumors. They arise from the supporting cells of the brain, called the glia. These cells are subdivided into astrocytes, ependymal cells and ologodendroglial cells (or oligos). Glial tumors include the following:
2) Astrocytomas are the most common glioma, accounting for about half of all primary brain and spinal cord tumors. Astrocytomas develop from star-shaped glial cells called astrocytes, part of the supportive tissue of the brain. They may occur in many parts of the brain, but most commonly in the cerebrum. People of all ages can develop astrocytomas, but they are more prevalent in adults, particularly middle-aged men. Astrocytomas in the base of the brain are more prevalent in children or younger people and account for the majority of children’s brain tumors. In children, most of these tumors are considered low-grade, while in adults most are high-grade.
3) Ependymomas are derived from a neoplastic transformation of the ependymal cells lining the ventricular system, and account for 2 to 3 percent of all intracranial tumors. Most are well-defined, but some are not.
4) Glioblastoma Multiforme (GBM) is the most invasive type of glial tumor. These tumors tend to grow rapidly, spread to other tissue, and have a poor prognosis. They may be composed of several different kinds of cells, such as astrocytes and oligodendrocytes. GBM is more common in people ages 50 to 70, and more prevalent in men than women.
5) Medulloblastomas usually arise in the cerebellum, most frequently in children. They are high-grade tumors, but they are usually responsive to radiation and chemotherapy.
6) Oligodendrogliomas are derived from the cells which make myelin, which is the insulation for the wiring of the brain.
Other types of Brain Tumors -
1) Hemangioblastomas are slow growing tumors that are commonly located in the cerebellum. They originate from blood vessels, can be large in size, and are often accompanied by a cyst. These tumors are more common in people ages 40 to 60, and more prevalent in men than women.
2) Rhabdoid Tumors are rare, highly aggressive tumors that tend to spread throughout the central nervous system. They often appear in multiple sites in the body, especially in the kidneys. They are more prevalent in young children, but can also occur in adults.
3) Pediatric Brain Tumors
Brain tumors in children typically come from different tissues than those affecting adults. Treatments that are fairly well tolerated by the adult brain (like radiation therapy) may prevent normal development of a child's brain, especially in children younger than age 5.
It is estimated that in 2005, 3,410 new cases of childhood primary nonmalignant and malignant brain and central nervous system tumors were diagnosed. Of these cases, an estimated 2,590 were in children 15 and younger.
Some types of brain tumors are more common in children than in adults. The most common types of pediatric tumors are medulloblastomas, low-grade astrocytomas, ependymomas, craniopharyngiomas, and brain stem gliomas.
A grading system is used to indicate how benign or how malignant a tumor is, basically in terms of the tumor’s histological features under a microscope. The World Health Organization (WHO) has developed the following brain tumor grading system:
World Health Organization (WHO) Brain Tumor Grades
LOW GRADE -
WHO Grade I - Characteristics
• Least malignant (benign)
• Possibly curable via surgery alone
• Non-infiltrative
• Long-term survival
• Slow growing
WHO Grade I - Tumor Types
• Pilocytic Astrocytoma
• Craniopharyngioma
• Gangliocytoma
• Ganglioglioma
WHO Grade II - Characteristics
• Relatively slow growing
• Somewhat infiltrative
• May recur as higher grade
WHO Grade II - Tumor Types
• "Diffuse" Astrocytoma
• Pineocytoma
• Pure oligodendroglioma
HIGH GRADE -
WHO Grade III - Characteristics
• Malignant
• Infiltrative
• Tend to recur as higher grade
WHO Grade III - Tumor Types
• Anaplastic astrocytoma
• Anaplastic ependymoma
• Anaplastic oligodendroglioma
WHO Grade IV - Characteristics
• Most malignant
• Rapid growth, agressive
• Widely infiltrative
• Rapid recurrence
• Necrosis prone
WHO Grade IV - Tumor Types
• Gliobastoma Multiforme (GBM)
• Pineoblastoma
• Medulloblastoma
• Ependymoblastoma
Brain Tumors Causes -
It is thought that brain tumors arise when certain genes on the chromosomes of a cell are damaged so that they no longer function properly. These genes normally regulate the rate at which the cell divides (if it divides at all), and repair genes that fix defects of other genes as well as genes that should cause the cell to self-destruct should the damage go beyond repair. In some cases, an individual may be born with partial defects in one or more of these genes. Environmental factors may then lead to further damage. In other cases, the environmental injury to the genes may be the only cause. It is not known why some people in an "environment" develop brain tumors while others do not.
Once a cell is dividing too rapidly and internal mechanisms to check its growth are damaged, the cell can eventually grow into a tumor. Another line of defense may be the body's immune system, which optimally would detect the abnormal cell and kill it. Tumors may produce substances that block the immune system from recognizing the abnormal tumor cells and eventually overpower all internal and external checks to its growth.
A rapidly growing tumor may need more oxygen and nutrients than can be provided by the local blood supply intended for normal tissue. Tumors can produce substances which promote the growth of blood vessels, called angiogenesis factors. The new vessels that grow increase the supply of nutrients to the tumor, and eventually the tumor becomes dependent on these new vessels. Research is being done in this area, but more extensive research is necessary to translate this knowledge into potential therapies.
Symptoms -
Symptoms vary depending on the location of the brain tumor, but the following are possible symptoms that may accompany different types of brain tumors.
• Headaches, which may be more severe in the morning
• Seizures or convulsions
• Difficulty thinking, speaking, or articulating
• Personality changes
• Weakness or paralysis in one part or one side of the body
• Loss of balance or dizziness
• Vision changes
• Hearing changes
• Facial numbness or tingling
• Nausea or vomiting
• Confusion and disorientation
Diagnosis -
Sophisticated imaging techniques can pinpoint brain tumors. Diagnostic tools include computed tomography (CT or CAT scan) and magnetic resonance imaging (MRI). Intraoperative MRI is also used during surgery to guide tissue biopsies and tumor removal. Magnetic resonance spectroscopy (MRS) is used to examine the tumor's chemical profile and determine the nature of the lesions seen on the MRI. Positron emission tomography (PET scan) can help detect recurring brain tumors.
Sometimes, the only way to make a definitive diagnosis of a brain tumor is through a biopsy. The neurosurgeon performs the biopsy and the pathologist makes the final diagnosis, determining whether the tumor appears benign or malignant, and grading it accordingly.
Brain Tumor Treatment -
Brain tumors (whether primary or metastatic, benign or malignant) are usually treated with surgery, radiation, and/or chemotherapy – alone or in variouscombinations. While it is true that radiation and chemotherapy are more often used for malignant, residual or recurrent tumors, decisions as to what treatment to use are made on a case-by-case basis and depend on a number of factors. There are risks and side effects associated with each type of therapy.
Surgery -
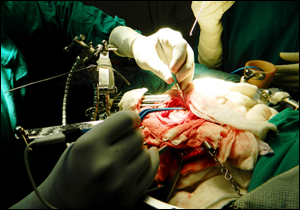
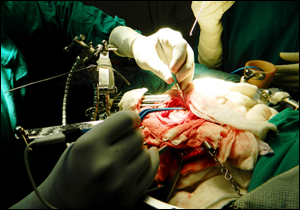
It is generally accepted that complete or nearly complete surgical removal of a brain tumor is beneficial for a patient. The neurosurgeon's challenge isto remove as much tumor as possible – without injuring brain tissue important to the patient's neurological function (such as the ability to speak, walk, etc.). Traditionally, neurosurgeons open the skull through a craniotomy, to insure that they can fully access the tumor and remove as much of it as possible.
Another procedure that is commonly done, sometimes before a craniotomy, is called a stereotactic biopsy. This is a smaller operation used to obtain tissue, so that an accurate diagnosis can be made. Usually, a frame is attached to the patient's head, a scan is obtained, and then the patient is taken to the operating area where a small hole is drilled in the skull to allow access to the abnormal area. A small sample is obtained, for examination under the microscope.
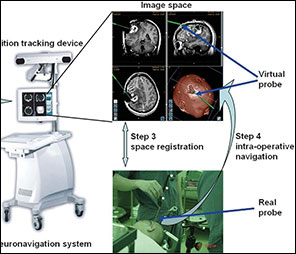
In the early 1990s, computerized devices called surgical navigation systems were first devised which eliminated the need for exploration. These systems assisted the neurosurgeon with guidance, localization and orientation. This information reduced the risks and improved the extent of tumor removal. In many cases, this allowed previously inoperable tumors to be excised with acceptable risks. Some of these systems can also be used for biopsies, without having to attach a frame to the skull. One limitation of these systems is that they utilize a scan (CT or MRI) obtained prior to surgery to guide the neurosurgeon. Thus, they cannot account for movements of the brain that may occur intraoperatively. Investigators are developing techniques using ultrasound, and performing surgery in MRI scanners, to help update the navigation system data during surgery.
Intraoperative language mapping is considered by some as a critically important technique for patients with tumors affecting language function, such as large, dominant-hemisphere gliomas. This procedure involves operating on an awake patient and mapping the anatomy of their language function during the operation, prior to deciding which portions of the tumor are safe to resect. Recent studies have determined that cortical language mapping may be used as a safe and efficient adjunct to optimize glioma resection while preserving essential language sites.
Ventriculo-peritoneal shunting may be required for some patients with brain tumors. Everyone has cerebrospinal fluid (CSF) within the brain (and spine) that is slowly circulating or flowing all the time. If this flow becomes blocked, the sacs that contain the fluid, the ventricles, can become enlarged, creating increased pressure within the head, called hydrocephalus. If left untreated, hydrocephalus can cause brain damage and even death. The neurosurgeon may decide to use a shunt to divert the spinal fluid away from the brain, and therefore reduce the pressure. The body cavity in which the CSF is diverted is usually the peritoneal cavity (the area surrounding the abdominal organs). The shunt is usually permanent. If it becomes blocked, the symptoms are similar to that of the original condition of hydrocephalus, and may include headaches, vomiting, visual problems, and/or confusion or lethargy, among others.
Complex Brain surgery using cutting edge technology -
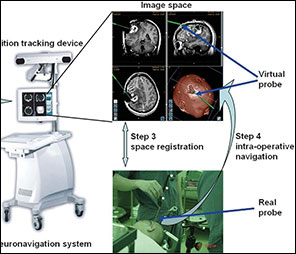
1. Computer guided Neuronavigation - the GPS of Brain Surgery—provides a window to operate on the brain by a minimal invasive microsurgical technique. This high precision method has made the removal of complex brain tumours more simple and safe , without harming the normal brain.
2. Image Guided Brain Surgery - using fluorescent dyes has enable complete tumour removal by advanced microsurgical method of fluorescence guided surgery.
3. Comprehensive Oncology Care - in adults & children- includes Neuro Oncology Surgery, Radiation Oncology, Medical Oncology, specialised Post operative Care, Neurorehabilitation, Home - Care; and long-term care with regular follow up in Oncology Clinics of AMRI hospitals.
4. A multidisciplinary multispecialty integrated treatment in AMRI Hospitals, ensures an enhanced quality of care required for a faster recovery and return to a normal life.
5. Specialised forms of radiation are also used to treat tumours directly using SRT, SRS after Neuronavigation guided stereotactic biopsy of tumours located deep inside the brain.
Radiation therapy uses high-energy x-rays to kill cancer cells and abnormal brain cells and shrink tumors. Radiation therapy may be an option if the tumor cannot be treated effectively through surgery.
1) Standard External Beam Radiotherapy uses a variety of radiation beams to create a conformal coverage of the tumor while limiting the dose to surrounding normal structures. The risk of long-term radiation injury with modern delivery methods is very low. Newer techniques of delivery aside from 3-dimensional conformal radiotherapy (3DCRT) include intensity-modulated radiotherapy (IMRT).
2) Proton Beam Treatment employs a specific type of radiation in which protons, a form of radioactivity, are directed specifically to the tumor. The advantage is that less tissue surrounding the tumor incurs damage.
3) Stereotactic Radiosurgery (like Gamma Knife, Novalis and Cyberknife) is a technique that focuses the radiation with many different beams on the target tissue. This treatment tends to incur less damage to tissues adjacent to the tumor. Currently, there is no data to suggest one delivery system is superior to another in terms of clinical outcome, and each has its advantages and disadvantage
Chemotherapy is generally considered to be effective for specific pediatric tumors, lymphomas and some oligodendrogliomas. While it has been proven that chemotherapy improves overall survival in patients with the most malignant primary brain tumors, it does so in only in about 20 percent of all patients, and physicians cannot readily predict which patients will benefit before treatment. As such, some physicians choose not to use chemotherapy because of the potential side effects (lung scarring, suppression of the immune system, nausea, etc.).
Chemotherapy works by inflicting cell damage that is better repaired by normal tissue than tumor tissue. Resistance to chemotherapy might involve survival of tumor tissue that cannot respond to the drug, or the inability of the drug to pass from the bloodstream into the brain. A special barrier exists between the bloodstream and the brain tissue called the blood-brain barrier. Some investigators have tried to improve the effect of chemotherapy by disrupting this barrier, or injecting the drug into the tumor or brain. The goal of another class of drugs is not to kill the tumor cells, but rather to block further tumor growth. In some cases, growth modifiers (such as Tamoxifen) have been used to attempt to stop the growth of tumors resistant to other treatments.
In 1996, a new method of delivering chemotherapy directly into the area of the tumor was approved by the U.S. Food and Drug Administration. This allows patients to receive chemotherapy without the systemic side effects. Chemotherapy-impregnated wafers can be applied by the neurosurgeon at the time of surgery. The wafers slowly secrete the drug into the tumor.
Many types of new therapies are currently being studied, especially for tumors for which the prognosis is generally poor through existing conventional therapies. It is unknown whether or not these therapies will work. Such therapies are given according to a "protocol", and include various forms of immunotherapy, therapy using targeted toxins, anti-angiogenesis therapy, gene therapy and differentiation therapy. Combinations of treatments may also be able to improve the outlook for patients, while lowering the adverse side effects.