Coronary artery disease, also called coronary heart disease, or simply, heart disease, is the No. 1 killer in America, affecting more than 13 million Americans.
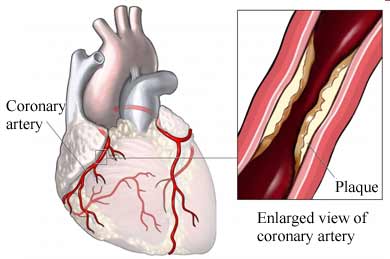
Heart disease is a result of plaque buildup in your arteries, which blocks blood flow and heightens the risk for heart attack and stroke.
What Is Coronary Artery Disease?
Heart disease is a result of plaque buildup in your coronary arteries -- a condition called atherosclerosis -- that leads to blockages. The arteries, which start out smooth and elastic, become narrow and rigid, restricting blood flow to the heart. The heart becomes starved of oxygen and the vital nutrients it needs to pump properly.
How Does Coronary Artery Disease Develop?
From a young age, cholesterol-laden plaque can start to deposit in the blood vessel walls. As you get older, the plaque burden builds up, inflaming the blood vessel walls and raising the risk of blood clots and heart attack. The plaques release chemicals that promote the process of healing but make the inner walls of the blood vessel sticky. Then, other substances, such as inflammatory cells, lipoproteins, and calcium that travel in your bloodstream start sticking to the inside of the vessel walls.
Eventually, a narrowed coronary artery may develop new blood vessels that go around the blockage to get blood to the heart. However, during times of increased exertion or stress, the new arteries may not be able to supply enough oxygen-rich blood to the heart muscle.
In some cases, a blood clot may totally block the blood supply to the heart muscle, causing heart attack. If a blood vessel to the brain is blocked, usually from a blood clot, an ischemic stroke can result. If a blood vessel within the brain bursts, most likely as a result of uncontrolled hypertension (high blood pressure), a hemorrhagic stroke can result.
What Is Ischemia?
Cardiac ischemia occurs when plaque and fatty matter narrow the inside of an artery to a point where it cannot supply enough oxygen-rich blood to meet your heart's needs. Heart attack can occur - with or without chest pain and other symptoms.
Ischemia is most commonly experienced during:
- Exercise or exertion
- Eating
- Excitement or stress
- Exposure to cold
Coronary artery disease can progress to a point where ischemia occurs even at rest. And ichemia can occur without any warning signs in anyone with heart disease, although it is more common in people with diabetes.
What Are the Symptoms of Coronary Artery Disease?
The most common symptom of coronary artery disease is angina, or chest pain. Angina can be described as a heaviness, pressure, aching, burning, numbness, fullness, squeezing or painful feeling. It can be mistaken for indigestion or heartburn. Angina is usually felt in the chest, but may also be felt in the left shoulder, arms, neck, back, or jaw.
Other symptoms that can occur with coronary artery disease include:
- Shortness of breath
- Palpitations (irregular heart beats, skipped beats, or a "flip-flop" feeling in your chest)
- A faster heartbeat
- Weakness or dizziness
- Nausea
- Sweating
How Is Coronary Artery Disease Diagnosed?
Your doctor can tell if you have coronary artery disease by:
- Talking to you about your symptoms, medical history, and risk factors.
- Performing a physical exam.
- Performing diagnostic tests, including an electrocardiogram (ECG or EKG), exercisestress tests, electron beam (ultrafast) CT scans, cardiac catheterization, and others. These tests help your doctor evaluate the extent of your coronary heart disease, its effect on the function of your heart and the best form of treatment for you.
Ho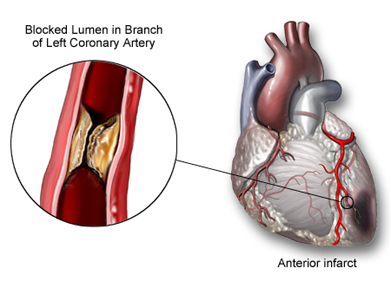 w Is Coronary Artery Disease Treated? w Is Coronary Artery Disease Treated?
Treatment for coronary artery disease involves making lifestyle changes, taking medications, possibly undergoing invasive and/or surgical procedures, and seeing your cardiologist for regular checkups.
Reduce your risk factors. If you smoke, quit. Avoid high-cholesterol foods and adopt a low-fat, low-salt diet. Keep your blood sugar in control if you have diabetes. Exercise more to maintain a healthy weight (but talk to your doctor before you starting an exercise program).
Medications. If making lifestyle changes isn't enough to control your heart disease, medications may be needed to help your heart work more efficiently and receive more oxygen-rich blood. The drugs you are on depend on you and your specific heart problem.
Surgery and other procedures. Common procedures to treat coronary artery disease include balloon angioplasty (PTCA), stent placement, and coronary artery bypass surgery. All of these procedures increase blood supply to your heart, but they do not cure coronary heart disease. You will still need to decrease your risk factors to prevent future disease.
Doctors are also studying several innovative ways to treat heart disease. Here are a couple of the more promising ones:
Angiogenesis. This involves giving substances, such as stem cells and other genetic material, through the vein or directly into damaged heart tissue to trigger the growth of new blood vessels to bypass the clogged ones.
EECP (Enhanced External Counterpulsation). Patients who have chronic angina but are not helped by nitrate medications or who do not qualify for various surgeries and procedures may find relief with EECP. The outpatient procedure involves using treatment cuffs placed on the legs that inflate and deflate, increasing the blood supply that feeds coronary arteries.
What to Do If You Have a Coronary Emergency?
Learn to recognize your heart disease symptoms and the situations that cause them. Call your doctor if you begin to have new symptoms or if they become more frequent or severe. If you or someone you are with experiences chest discomfort, especially if there is shortness of breath, heart palpitations, dizziness, a fast heart beat, nausea or sweating, don't wait longer than a few minutes to call 911 for help.
If you have angina and have been prescribed nitroglycerin, call your doctor or have someone take you to the nearest emergency room if pain persists after taking two doses (taken at five-minute intervals) or after 15 minutes.
Emergency personnel may tell you to chew an aspirin to help break up a possible blood clot, if there is not a medical reason for you to avoid aspirin. |