• HYSTEROSCOPY:
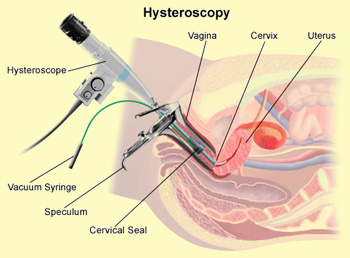
Hysteroscopy, is a procedure where the inside of the cervix and uterus is visualized using a camera attached to the TV monitor. Two types of the procedure are generally performed: diagnostic and operative hysteroscopy.
1. Diagnostic hysteroscopy allows the visualization of the inside of the uterus and diagnosis of such common conditions as fibroids, uterine polyps, uterine septum, etc.
During the procedure, which can be done either in the office settings under local anesthesia or in the operating room under general anesthesia, the camera (hysteroscope) is placed through the vagina and the cervix into the uterus. In majority of cases, there is no need to dilate (open) the cervix. The inside of the uterine cavity is examined and problems, if any, are noted. In cases of abnormal uterine bleeding, a physician can choose to take a sample of the endometrial lining utilizing tiny suction tube.
2. Operative hysteroscopy is usually done in the operative room under general anesthesia. This procedure is reserved for patients with known intrauterine pathology such as previously diagnosed fibroids that may cause bleeding and infertility, uterine polyps, uterine septum, blocked Fallopian tubes, etc.
The cervix will need to be slightly dilated to allow the passage of the operative hysteroscope inside the uterus. Sterile fluid is also infused into the uterus to allow for better visualization. Certain types of fibroids, polyps, or any other defects can be treated and removed by using electrical and mechanical hysteroscopic instruments. Very often the biopsy of the endometrial lining is performed at the same time (known as D & C).
One of the subtypes of the operative hysteroscopy is a procedure known as endometrial ablation. Endometrial ablation is indicated in women who have finished their reproductive years and have heavy and/or irregular bleeding. After uterine cancer as a cause of bleeding is ruled out, which is often done by the in-office diagnostic hysteroscopy, the endometrial ablation can be performed. Result of multiple studies has shown very good outcomes and satisfaction among women who underwent endometrial ablation.
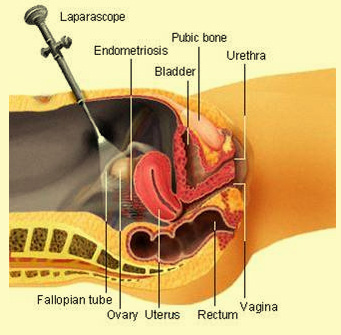
In complicated cases of pelvic pain and/or infertility, a physician might choose to perform hysteroscopy together with laparoscopy (looking inside your abdomen and pelvis).
Hysteroscopy is a procedure that involves insertion of a narrow telescope-like instrument through the vagina and cervix into the cavity of the uterus (endometrial cavity). The uterine cavity is then distended with fluid and visualized.
 What is hysteroscopy used for? What is hysteroscopy used for?
This procedure allows us to see if there are any uterine cavity defects such as:
- Fibroid tumors
- Endometrial polyps
- Intrauterine scar tissue
- A bicornuate uterus or septate uterine malformation
- Other uterine problems
If any defects are found then they should be corrected with operative hysteroscopy which involves placing instruments through ports in the scope that allow us to cut, cauterize, etc. to correct the problem.
About hysteroscopy
Hysteroscopy procedure can help find out what's causing symptoms such as unusual vaginal bleeding or discharge. It can also be used to check for certain womb conditions such as polyps (small growths of tissue in the womb lining), fibroids (non-cancerous growths of muscle in the womb), heavy periods or early signs of womb cancer.
During the procedure your surgeon may take a biopsy (a small sample of tissue) for examination in a laboratory, and/or treat the inside of your womb. It's also possible to remove polyps that may be found on your womb lining, as well as scar tissue and intra-uterine contraceptive devices (IUCDs) or "coils" that have become lost or stuck.
What are the alternatives?
Depending on your symptoms and circumstances, it may be possible to examine your womb using pelvic ultrasound. This is a technique that uses sound waves to produce an image of the inside of your womb.
A simpler procedure, called endometrial aspiration, may be another alternative to a hysteroscopy and your surgeon will advise if this is suitable for you. This involves passing a narrow tube through your cervix and into your womb, and uses suction to remove samples of your womb lining. For most women, however, a hysteroscopy is the best option to help diagnose or treat the problem. Unlike other tests, it enables your surgeon to see directly into your womb.
Preparing for your hysteroscopy
Hysteroscopy is routinely done as an out-patient or day case and your surgeon will explain how to prepare for your procedure.
Hysteroscopy can be performed with or without a local anaesthetic, especially if it's only being used for a check-up (called a diagnostic hysteroscopy). A local anaesthetic completely blocks feeling from the area around your womb and you will stay awake during the procedure. Sometimes it's done under general anaesthesia, usually to treat a medical condition or to take a biopsy (called an operative hysteroscopy). This means you will be asleep during the procedure. Your surgeon will advise which type of anaesthesia is most suitable for you.
If you are having a local anaesthetic there is no need to go without food or drink before your hysteroscopy. If you are having a general anaesthetic, you will be asked to follow fasting instructions. Typically you must not eat or drink for about six hours before a general anaesthetic, although you will be allowed occasional sips of water until two hours beforehand.
At the hospital your nurse may do some tests such as checking your heart rate and blood pressure, and testing your urine.
You may be asked to sign a consent form. This confirms that you understand the risks, benefits and possible alternatives to the procedure and have given your permission for it to go ahead.
About the procedure
 The procedure usually takes about 10 minutes to over half an hour, dependingon what needs to be done. The procedure usually takes about 10 minutes to over half an hour, dependingon what needs to be done.
Your surgeon may use a speculum to gently open your cervix (similar to having a smear test). The speculum is a device that's inserted into the vagina to help view the cervix. Your surgeon will clean your vagina and cervix with an antiseptic solution and pass the hysteroscope through the cervix and into your womb. He or she may pump gas or fluid into your womb to make it expand. This makes it easier to see the womb lining.
The camera at the end of the hysteroscope sends pictures from the inside of your womb to a video screen. Your doctor will look at these images and if necessary take a biopsy, remove polyps, and/or deliver treatment. This is done using special instruments passed inside the hysteroscope, and it's usually quick and painless.
When the examination is finished, the hysteroscope is gently taken out.
What to expect afterwards
If you have a biopsy or polyps removed, you may need to wear a sanitary towel to absorb any vaginal bleeding.
If you have a local anaesthetic, you will usually be able to go home after a short rest.
If you have general anaesthesia, you will need to rest until the effects of the anaesthetic have passed. You will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours.
Results
If you have a biopsy or polyps removed, the results will be ready several days later and will usually be sent in a report to the doctor who recommended your test. Other findings may be discussed before you leave the hospital.
If you have general anaesthesia, it's a good idea to have someone with you if the results are being discussed immediately after the procedure, as you may not remember the details clearly.
Recovering from your hysteroscopy
General anaesthesia can temporarily affect your coordination and reasoning skills, so you should not drive, drink alcohol, operate machinery or sign legal documents for 48 hours afterwards. If you are in any doubt about driving, please contact your motor insurer so that you are aware of their recommendations, and always follow your doctor's advice.
If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Follow the instructions in the patient information leaflet that comes with the medicine and ask your pharmacist for advice.
It's important to take it easy for the rest of the day. Some women feel ready to return to normal activities and work the day after the procedure; others may need to take two or three days off. Follow your doctor's advice about exercise, having sex and contraception.
You shouldn't use tampons for at least one month after your hysteroscopy to help reduce the risk of infection.
You may find that your first period following the hysteroscopy is heavier or more prolonged than usual and that your periods are irregular for a couple of months.
Most women don't have any problems after having a hysteroscopy. However, please contact your doctor if you develop:
- prolonged heavy bleeding
- vaginal discharge that is dark or smells unpleasant
- severe pain or pain that lasts for more than 48 hours
- a high temperature
What are the risks of hysteroscopy?
Hysteroscopy is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side Effects
Side-effects are the unwanted, but mostly temporary effects of a successful procedure. After a hysteroscopy you may:
- have slight period-like cramps and may need painkillers
- feel some pain in the tip of your shoulders caused by the gas or fluid used to inflate the womb - this usually clears up with 48 hours
- have some vaginal bleeding and discharge - this usually clears after a few days but can last up to several weeks
Complications
This is when problems occur during or after the procedure. Most women are not affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (deep vein thrombosis, DVT).
Specific complications of hysteroscopy are uncommon but it's possible to:
- develop a pelvic infection afterwards, needing treatment with antibiotics
- damage or perforate the womb during the procedure - this can lead to bleeding and infection, which may require further surgery
Your surgeon will be experienced at performing hysteroscopies. Rarely, this procedure isn't successfully completed and may need to be repeated.
The exact risks are specific to you and will differ for every woman
Is it a big procedure? How much work would I miss?
Hysteroscopy is an out-patient procedure that is usually done in a hospital but can also be done in the office. The actual procedure (diagnostic) usually takes 2-5 minutes. No anesthesia at all is needed for most cases of diagnostic hysteroscopy if a microhysteroscope (scope diameter less than 5mm) is used. General anesthesia or local anesthesia can be used if any operative work is required. Usually the woman is discharged home approximately 15-30 minutes after the procedure. She can return to work the next morning if general anesthesia was used, or immediately if no anesthesia (or local) was used. Mild pain and cramping is common after operative hysteroscopy, but it usually is brief (lasting perhaps 30 minutes, possibly up to 8 hours).
What problems can defects of the uterine cavity cause?
Abnormalities of the endometrial cavity can be responsible for infertility or problems with recurrent miscarriage.
Hysteroscopy and other methods, such as a hysterosalpingogram, ultrasound, or ultrasound with saline test are useful in diagnosing and correcting these defects..
Approximately 20% of Indian couples experience difficulty in their attempts to achieve pregnancy. There are many and various factors that may contribute to infertility. An infertility work-up by a medical fertility specialist is necessary to determine the specific cause and subsequent treatment. The linked list to the right includes important information specific to some of the options that may assist you in preparing for your assessment. |