Laparoscopic and minimally invasive surgery has become the mainstream in operating rooms across India. The field of gynecologic surgery is clearly not an exception, as minimally invasive gynecology has gained enormous momentum within the specialty.
Advances in computer technology and laparoscopic instruments have allowed us to offer a minimally invasive approach to a much broader range of patients. The field of gynecologic surgery is proudly included in this medical and surgical marvel.
As of today, many procedures can be successfully done by a minimally invasive approach in most patients including:
- Hysterectomy (removal of the uterus)
- Oophorectomy (removal of the ovaries)
- Myomectomy (removal of the fibroids)
- Treatment of endometriosis and pelvic pain
Treatment of abnormal uterine bleeding and hysteroscopy (the visualization of the inside of the uterus), myomectomy (removal of uterine myomas), cervical stenosis, and sacrocolpopexy (treatment of the prolapse of the vagina) and treatment of pelvic pain are among his areas of expertise.
Dr. Abhinibesh Chatterjee and Dr Polly Chatterjee has published scientific papers and presented at multiple national and international meetings.
• LAPAROSCOPY:
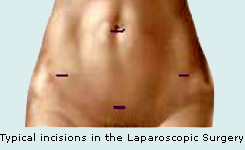
Laparoscopy, a surgical technique where a small camera, usually between 5 and 10 mm (less than ½ inch), is inserted into a patient’s abdomen for the purpose of the visualization of the pelvic and abdominal anatomy, diagnosis of a disease condition, and treatment of such condition by a minimally invasive approach. Several small incisions (less than ¼ inch) are made in the bikini line for the introduction of laparoscopic instruments, such as laparoscopic scissors, scalpel, etc.
Multiple gynecologic procedures and surgeries that are routinely done by an open technique can be potentially done by laparoscope, including:
- Removal of the uterus (Laparoscopic Hysterectomy)
- Removal of the fibroids (Laparoscopic Myomectomy)
- Surgical treatment of ovarian cysts (Laparoscopic Cystectomy)
- Ectopic pregnancy
- Treatment of endometriosis and pelvic pain (Laparoscopic Presacral Neurectomy)
These are just a few examples of the laparoscopic surgeries in the field of gynecology.
There are a number of advantages to the patient with laparoscopic surgery versus an open procedure:
- Smaller incisions, leading to shorter recovery time and less post-operative pain
- Less pain medication needed due to less post-operative pain.
- Reducing blood loss, potentially lowering the the chance of needing a blood transfusion
- Shorter hospital stays, and often with a same day discharge.
- Reduced exposure of internal organs, thus reducing the risk of infection.
.
• HYSTEROSCOPY:
Hysteroscopy, is a procedure where the inside of the cervix and uterus is visualized using a camera attached to the TV monitor. Two types of the procedure are generally performed: diagnostic and operative hysteroscopy.
1. Diagnostic hysteroscopy allows the visualization of the inside of the uterus and diagnosis of such common conditions as fibroids, uterine polyps, uterine septum, etc.
During the procedure, which can be done either in the office settings under local anesthesia or in the operating room under general anesthesia, the camera (hysteroscope) is placed through the vagina and the cervix into the uterus. In majority of cases, there is no need to dilate (open) the cervix. The inside of the uterine cavity is examined and problems, if any, are noted. In cases of abnormal uterine bleeding, a physician can choose to take a sample of the endometrial lining utilizing tiny suction tube.
2. Operative hysteroscopy is usually done in the operative room under general anesthesia. This procedure is reserved for patients with known intrauterine pathology such as previously diagnosed fibroids that may cause bleeding and infertility, uterine polyps, uterine septum, blocked Fallopian tubes, etc.
The cervix will need to be slightly dilated to allow the passage of the operative hysteroscope inside the uterus. Sterile fluid is also infused into the uterus to allow for better visualization. Certain types of fibroids, polyps, or any other defects can be treated and removed by using electrical and mechanical hysteroscopic instruments. Very often the biopsy of the endometrial lining is performed at the same time (known as D & C).
One of the subtypes of the operative hysteroscopy is a procedure known as endometrial ablation. Endometrial ablation is indicated in women who have finished their reproductive years and have heavy and/or irregular bleeding. After uterine cancer as a cause of bleeding is ruled out, which is often done by the in-office diagnostic hysteroscopy, the endometrial ablation can be performed. Result of multiple studies has shown very good outcomes and satisfaction among women who underwent endometrial ablation.
In complicated cases of pelvic pain and/or infertility, a physician might choose to perform hysteroscopy together with laparoscopy (looking inside your abdomen and pelvis).
• LAPAROSCOPIC HYSTERECTOMY:
Hysterectomy, the surgical removal of the uterus, is a recommended intervention in variety of gynecologic conditions, including:
- Abnormal excessive bleeding
- Fibroids
- Uterine cancer
- Cervical cancer
- Endometriosis and adenomyosis (in some cases)
These are just a few of many conditions that might require a hysterectomy.
Typically, depending on whether the condition is benign (such as fibroids or pain) or malignant (such as cancer), either a total hysterectomy with the removal of the body of the uterus together with the cervix, or subtotal/partial hysterectomy (the cervix is left behind) is performed. Removal of the ovaries at the time of hysterectomy is very controversial topic and should be discussed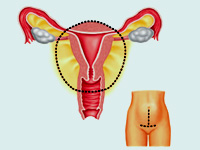 individually in every case. individually in every case.
In the past, the only available option for hysterectomy was an open abdominal surgery.
The incision would be made in either “bikini” or up-and-down fashion, the uterus would be removed, and abdomen closed in multiple layers with sutures and staples.
Typically, a woman would spend 5 to 7 days in the hospital with several months of recovery at home. In addition, the surgery would leave a large scar on the abdomen.
 With the advent of better optics and laparoscopic instruments, the era of laparoscopic hysterectomy came to age. Utilizing magnified surgical field and available electrosurgical and ultrasonic instruments, the removal of the uterus is achieved through several (usually 3 to 4) ½ to ¼ inch incisions. Minimal blood loss and fast recovery time are the major advantages of laparoscopic hysterectomy, not to mention excellent cosmetic results. Most women go home either the same or next day and fully on their feet within a week or two. With the advent of better optics and laparoscopic instruments, the era of laparoscopic hysterectomy came to age. Utilizing magnified surgical field and available electrosurgical and ultrasonic instruments, the removal of the uterus is achieved through several (usually 3 to 4) ½ to ¼ inch incisions. Minimal blood loss and fast recovery time are the major advantages of laparoscopic hysterectomy, not to mention excellent cosmetic results. Most women go home either the same or next day and fully on their feet within a week or two.
These are the few of the benefits of the Laparoscopic Hysterectomy:
- Decreased blood loss
- Faster recovery time
- Greatly reduced post-operative pain
- Quicker return to daily activities
- Improved cosmesis
• LAPAROSCOPIC ADNEXAL SURGERY:
Laparoscopic adnexal surgery is a minimally invasive procedure done on the ovary, fallopian tube, or ovarian cysts.
Reasons for the procedure:
Different circumstances sometimes make it necessary remove one or both ovaries or the fallopian tube such as:
- Bleeding ectopic pregnancy
- Ovarian malignancy
- Ectopic pregnancy or inflammation of the fallopian tube
- Ovarian cysts -- often, it is necessary to remove one or more ovarian cyst (ovarian cystectomy) due to pain, cyst rupture, or the possibility of cancer.
Sometimes, the cause of infertility can be diagnosed and treated surgically on the fallopian tubes (such as breaking down the adhesions that prevent the fertilization of the egg).
All of these procedures can be performed laparoscopically.
• How the procedure is done
The surgery involves making the small incision in the belly button through which the camera (laparoscope) is inserted, allowing direct, thorough, and magnified evaluation of pelvic and abdominal organs. Three tiny incisions are made in the bikini line to allow introduction of laparoscopic instruments.
• Advantages of minimally invasive surgery
This minimally invasive approach reduces exposure of internal organs, minimizing the chance of infection. It also reduces the amount of blood loss, thus reducing the need for potential blood transfusion.
Because there are no large incisions, the recovery time is much shorter: most people go home the same day or the morning after the surgery. In majority of cases, full recovery takes around one week. And there are no or minimally visible scars left after laparoscopic procedure.
• LAPAROSCOPIC PRESACRAL NEURECTOMY (LPSN):
Presacral Neurectomy is the surgical removal of the presacral plexus – the group of nerves that conducts the pain signal from the uterus to the brain. Indicated for the treatment of central pelvic pain including severe dysmennorrhea
Laparoscopic Presacral Neurectomy (LPSN) is the same procedure done by a minimally invasive method. It is a surgical approach in patients with central dysmenorrheal (painful periods), adenomyosis, and endometriosis.
• How the procedure is done
Done through a small umbilical and bikini line incisions, LPSN is carried out by removing the nerve fibers that innervate the uterus, thus blocking the pathways for pain impulses to the brain. LPSN does not cure the pelvic pain that is lateral, which is related to the ovarian or other pelvic sidewall structures.
When performed correctly and in the appropriately chosen patient, the complications PSN are minimal and sometimes include constipation, urinary symptoms, or painless labor.
• About Central Pelvic Pain
Central pelvic pain (CPP) is reported in about 20 percent of menstruating females. Chronic pelvic pain refers to menstrual or non-menstrual pain of at least six months’ duration.
Dysmenorrhea, one of the most frequently reported gynecological problems, is characterized by sharp, intermittent spasms. Symptoms of headache, nausea, vomiting, diarrhea and fatigue are also present. Pain typically begins before or at the onset of menses.
The prevalence of the disorder is highest in adolescents with estimates ranging from 20–90 percent.
Risk factors for the disorder include nulliparity, heavy menstrual flow, smoking, and depression. Medical therapy for dysmenorrhea includes NSAIDs (such as Motrin) and/or oral contraceptives. Approximately 10–25% of women with dysmenorrhea do not respond to medical management and may require surgical intervention, such as presacral neurectomy.
Strict selection of patients and adherence to the established protocol are the requirements for the successful presacral neurectomy (PSN), leading to the reported cure rates between 65 and 80 percent.
Laparoscopic Myomectomy Frequently Asked Questions (FAQs):
If you or someone you know has recently been diagnosed with uterine fibroids and are searching for an alternative to a traditional hysterectomy, you might consider asking your surgeon if you could be a candidate for a laparoscopic myomectomy.
Laparoscopic myomectomy help patients get on the road to a quicker recovery with significantly less pain and fewer future complications.
Click on any of the questions listed below, or simply scroll down the page to find answers to some commonly asked questions about this surgical technique.
• What are uterine fibroids?
Uterine fibroids are non-cancerous (benign) tumors that develop within the uterus. Symptoms usually include heavy menstrual bleeding, pelvic pain and infertility, making them the leading cause of hysterectomies performed in the United States.
Uterine fibroids usually occur in women over 30 years of age, and are rarely diagnosed in women younger than 20. These benign growths are quite common, occurring in approximately one-third of all women.
• What is laparoscopic myomectomy?
Surgeons remove fibroids while preserving the patient’s uterus. The procedure begins with an examination of the uterus and fibroids. The surgeon controls the laparoscopic instruments attached to the surgical system. These instruments act as a computerized extension of the surgeon’s hands, allowing the surgeon to separate the fibroids from the uterus and restore the patient’s anatomy with unmatched surgical precision.
• How does a laparoscopic myomectomy differ from traditional open surgery?
A myomectomy performed through open surgery requires a large incision into the patient’s abdomen, cutting through layers of skin and muscle in order to reach the affected area. This incision leaves patients with a large scar and varying amounts of abdominal muscle weakness following the procedure. Open surgery also increases the length of time needed for recovery and the risk for infection.
Laparoscopic myomectomy helps surgeons overcome many of the challenges associated with the removing uterine fibroids. It affords surgeons a great level of precision and control when using its instruments. Potential uterine bleeding, infections and scarring are minimized.
• What are the benefits for the patient?
A laparoscopic myomectomy offers several benefits to the patient, including:
- Fewer surgical complications
- Less blood loss
- Minimal scarring
- Opportunity for future pregnancy
- Quicker recovery
- Shorter hospital stay
- Significantly less pain
• Why come to Dr Abhinibesh Chatterjee and Dr Polly Chatterjee?
Offers compassionate care from physicians with advanced surgical skills who have access to technology available at only a handful of medical centers in the country. Because there is no one type of surgery that is appropriate for all patients, we provide a variety of surgical options for patients in need of traditional and advanced surgical procedures. Patients have access to a multi-disciplinary treatment team who will help them formulate individualized treatment plans depending upon their specific condition, complaints, and preferences. This patient-centered treatment approach assures the most comprehensive and integrated care for your uterine fibroids.
Frequently Asked Questions Laparoscopic Surgery for Prolapse :
Used in the early 20th century to treat rectal prolapse, the Moschcowitz Procedure has since been adapted by gynecologists in the treatment of vaginal prolapse, particularly for women who have had a hysterectomy.
• What are the causes of vaginal prolapse?
The complex interplay of factors during the development of the vagina and the rectum while the baby in the uterus, as well as factors later in life such as multiple vaginal births, chronic constipation, chronic cough and repetitive heavy lifting are all contributors to the development of the vaginal prolapse.
• What is the Moschcowitz Procedure?
The Moschcowitz Procedure was originally described by Alexis Moschcowitz in 1911 for the treatment of rectal prolapse or "the rectal hernia." Dr. Moschcowitz's ground-breaking approach stemmed from the understanding of principles of embryonic development and normal anatomy. His surgical method of elevating the rectum and closing of the sac between the rectum and the vagina was soon adapted by gynecologists for the treatment of vaginal prolapse, particularly after hysterectomy.
• How is the Moschcowitz procedure performed?
In the past, the Moschocowitz procedure was done primarily by open route. With the ability of the laparoscopic arms to provide enhanced manipulation of the surgical instruments and suturing techniques, it now can be performed in a minimally invasive manner. This approach reduces post-operative pain, improves surgical cosmesis and assures better surgical techniques.
• When is the Moschcowitz procedure performed?
The procedure is performed in a minimally invasive approach right after completion of a total hysterectomy (removal of the uterus and the cervix). The goal of the Moschcowitz procedure is to fix and suture the strong connective tissue that normally supports the uterus to the top of the vagina, thus preventing it from "falling out." At the same time, the pouch between the rectum and the vagina is reduced with a purse-string type suture.
Surgical Treatment of Pelvic Endometriosis
• What is endometriosis?
Endometriosis is a condition in which the tissue normally found inside the uterus (the endometrium) begins to grow outside of the uterus – on the bladder, ovaries, bowel and pelvic sidewall.
• What are the typical symptoms of pelvic endometriosis?
Although symptoms may vary from woman to woman, classical presentation of pelvic endometriosis includes:
- Severe menstrual cramps and pain
- Pain during sex
- Persistent pelvic pain
- Pain with urination and bowel movements, especially around the period
- Infertility
• What causes endometriosis?
The scientific community is still debating the true cause of pelvic endometriois. One widely accepted theory is “Retrograde Menstruation”, which posits that, during menstrual bleeding, blood with endometrial tissue gets into the pelvis and the abdomen. If not cleared by body’s immune system, the endometrial tissue becomes implanted on the other organs (such as the ovaries). That tissue then “bleeds” under hormonal influence, causing pain during each menstrual cycle.
Other theories, such as genetic predisposition to endometriosis, autoimmune dysfunction, environmental theory and others also exist. In reality, the development of pelvic endometriosis is probably the result of multiple mechanisms, including those mentioned above.
• How is pelvic endometriosis treated?
There are several medical (conservative) treatment options available. Hormone therapy (HT) in the form of an injection, pill or IUD are the first line of management. Unfortunately, in many cases, medical treatment is inadequate at controlling symptoms of pelvic endometriosis. In those cases, surgical management is the only option.
• How is surgery performed?
In the majority of cases, surgical management of pelvic endometriosis is performed through a minimally invasive approach – several 5 to 10 mm (1/3 of an inch) incisions are made, and the abdomen and pelvis are examined under high magnification with the laparoscope.
The endometriotic tissue is removed with the help of tiny scissors, lasers or electrosurgery (burning). Some tissue samples are sent to the laboratory to confirm the presence of the disease.
In severe cases of endometriosis, which involve the bladder or bowel, consultation with a urologist and/or colorectal surgeon is needed. After surgery, you will be placed on a comprehensive therapy regimen. |