| |
| Treatment & Surgery ... |
| |
Cataract Unit
What is Cataract?
Normally, the lens of the eye is clear and allows light rays to pass through easily. When a cataract develops, the lens becomes cloudy and opaque. The light rays no longer pass through the lens easily, so the patient cannot see clearly.
- Cataract is not a new growth or a film over the eye. In most cases, it is just part of the aging process.
- It is not contagious
Types of Cataract
There are many types of cataracts.
A change in the chemical composition of the lens causes most cataracts. The following are the various types of cataracts.
- Senile Cataract
This is the most common type of cataract, comprising 80 percent of the total cataracts. It occurs in patients above the age of 50.
- Congenital Cataract
Cataracts in children are rare. They can be caused by infection of the mother during pregnancy, or they may be hereditary.
- Traumatic Cataract
Eye injuries may cause cataracts in patients of any age.
- Secondary Cataract
Eye diseases, like glaucoma, iritis, eye tumours, and diabetes may cause cataracts.
- Drug-induced Cataract
Prolonged treatment with steroid drugs, either for local (e.g., allergic conjunctivitis) or systemic diseases (e.g., asthma) may lead to cataract formation.
- Symptoms of Cataract
Cataract formation is not associated with "signals" such as pain, redness or tearing. The common symptoms are:
 |
 |
| (i) Blurring or dimness of vision |
(ii) Feeling of a film over the eyes |
 |
 |
| (iii)Sensitivity to light and glare |
|
 |
 |
| (iv) Change in colour of pupil |
Double vision & dulling of colour sens |
Treatment
Cataract cannot be cured by medicines or spectacles. Removal of the clouded lens through surgery is the only treatment.
Types of Cataract Removal:
Routine method (old method)
After administering a local anesthesia, a 10 mm incision is made in the eye. The cataract lens is removed and it may be replaced by an Ophakic glass. The incision is then closed with sutures. After the surgery, glasses with high power called ophakic spectacles are prescribed to the operated person.
Disadvantages:
These ophakic glasses are heavy, images seen are larger than they normally appear to be, and the field of vision is restricted.
What is IOL?
Intra Ocular lens (IOL) is a tiny transparent convex lens. It is made of polymethyl methacrylate,
(a harmless plastic substance).
Unlike contact lens, an IOL stays permanently in the eye and does not cause irritation.
Advantages of IOL:
- Since the lens is placed inside the eye, most often the patient need not wear glasses for clear vision. But sometimes patient has to wear glasses for clarity.
- Images are clear and of the same dimension without distortion
- Full vision returns very clearly
- Normal field of vision
New method with implanting of Intraocular lens (IOL) with sutures:
After administering a local anesthesia, a 10 mm incision is made in the eye. The clouded lens is removed and replaced by an IOL and the incision is then closed with sutures. The entire procedure takes only 15 minutes.
Phaco or suture less surgery with implantation of IOL
After giving a local anesthesia, a 5mm incision is made in the eye. The cataract lens is broken into small pieces by a machine with ultrasonic waves and removed with a needle. A specially prepared IOL is inserted into the eye and the wound heals without sutures.
Advantages of Phaco
- Early surgery can be done, so that patient need not wait for the cataract to mature
- Small Incision
- No sutures and no need of suture removal.
- No irritation, no watering
- Early return to work
- No need to continue drops for a long time
- No need for hospital stay, Even if the patient stays, it is only for a short time
- Only one post-operative visit
- Stable refraction after one month
The ophthalmic surgeon decides whether the patient can undergo phaco or not. |
| |
|
| |
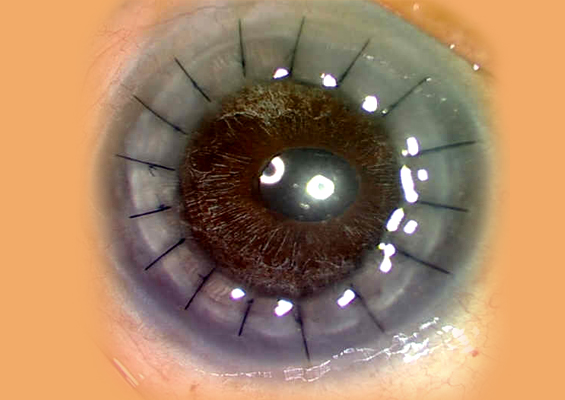
CORNEAL BLINDNESS |
The clear and transparent front portion of the eyeball wall is Cornea. Maintaining
transparency is the main function of Cornea, allowing external light to enter eyeball
without any obstruction, beside contributing some focusing power to the vision
apparatus.
Therefore any opacity, irregularity or abnormal change of corneal curvature can interfere
with these function resulting in poor vision or corneal blindness.
Corneal opacity can be caused by injury, ulcer infective or non infective, degeneration
abnormal development, surgery etc. A normal curvature change may be due to
keratoconus, corneal scar or may be surgically induced.
Abnormal curvature change and irregularity of corneal surface interfere with focussing
function of cornea, which may be corrected by proper glasses, contact lenses or lasik
laser surgeries or corneal transplantion.
Ulcer may be of bacterial, viral, fungal or amoebie in origin. " Viral ulcer" may be
recurrent, while fungal and amoebie are less responsive to medical treatment than
bacterial one. Any Corneal ulcer is a semi emergency, and needs prompt medical therapy
to achieve quick healing to limit the seize and density of scar that will be left behind
permanently. In non responding cases one may need therapeutic Corneal transplantation
just to save the eyeball ( by giving mechanical support to sloughing out Cornea). Such
transplanted cornea usually becomes opaque but later on a second transplantation may be
done for restoring vision.
Any significant Corneal opacity resulting from various condition needs Corneal
transplantation. A doner clear Cornea is collected from cadaver within six hour of death
which is processed in an eye bank and stored in a special medium for preservation. Such
Cornea will be used for Corneal transplantation for needy patient suffering for Corneal
blindness.
Corneal transplantation can restore normal or useful vision to such patients. Like any
other organ transplantation, Corneal transplantation is not without the risk of rejection
The risk of rejection is much less in case of Cornea as it is a blood less structure.
Majority cases of rejection can be managed and clarity can be maintained if patient
reports early any redness and blurring of vision. Patient compliance for follow up is the
major factor in good outcome of Corneal transplantation surgery. |
| |
|
| |
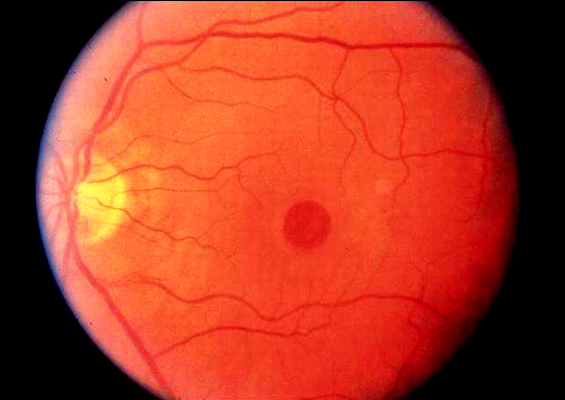
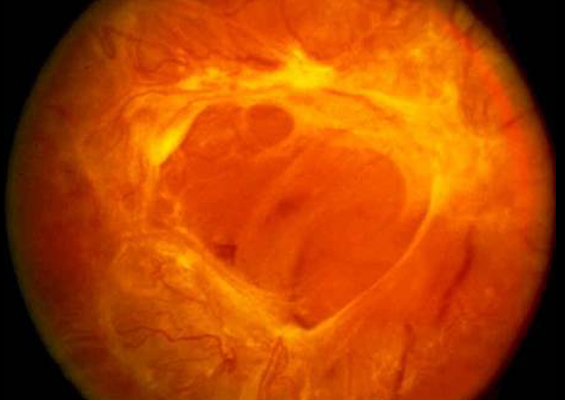
| Retina |
Debipur Netralaya Provides facilities for (1) Retinal Examination like I/O. 90-D Exam, 78-D Exam, D.F.A etc and (2) Treatment of Retinal Pathologies like green Laser PHC, Cryoretinopexy, Scleral Buckling Operation, Vitrectromy Surgery ( Selected Cases) etc. |
| |
 |
 |
 |
 |
Appa Brilliant Surgical
Microscope |
Double Beded Operation
Theatre |
Running Cataract Surgery |
Cleaning and Rectus Before
Surgery |
 |
 |
 |
 |
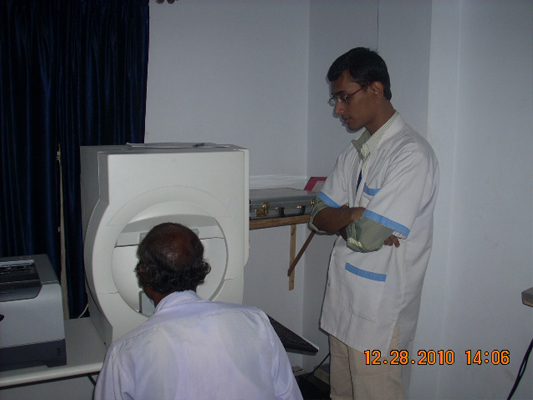
Field of Vision Test By
Humpherey Perimetry |
Details History of Congenital
Blind Patient have taken By
Optometrist |
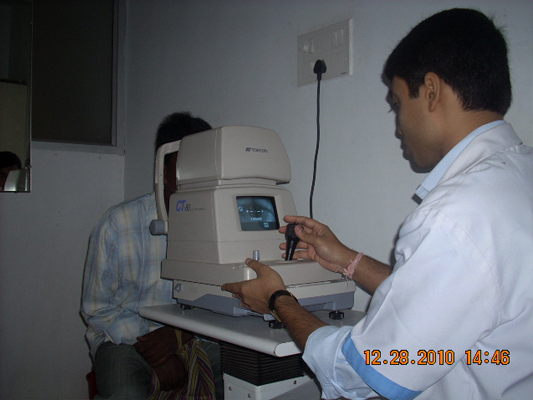
IOP By Topcon NCT or Airpuff Tonometer |
Anterior & Partial Posterior
Segment Examination By
Opthalmologist |
 |
 |
 |
 |
| Use of Pinkey |
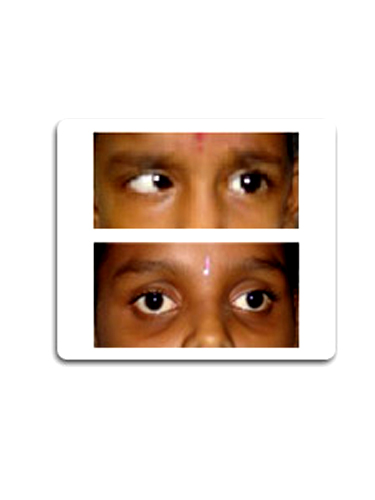
Child Surgery |
Squint |
Retinal Hole |
 |
 |
 |
 |
| Cloudy Cornea |
Cornea Transplant (Redial Keratoplasty) |
Cornea Transplant |
Exudative Retinal Detachment |
 |
 |
 |
 |
| Retinal Hole 2 |
A Handicapped Patient
Come Out from Out |
Squint Surgery |
Tumour (Ocuplasty SX.) |
|
| |
| Squint |
| |
What is squint (strabismus)?
Squint is a misalignment of the two eyes where in two eyes are not looking in the same direction.
This misalignment may be constant, being present throughout the day, or it may appear sometimes and the rest of the time the eyes may be straight called as intermittent squint.
What causes squint?
The exact cause of squint is not known. Six external eye muscles control the movement of each eye . Each of these muscle acts along with its counterpart in the other eye to keep both the eyes aligned properly. A loss of coordination between the muscles of the two eyes leads to misalignment. Sometimes a refractive error e.g. hypermetropia (far sightedness) or an eye muscle paralysis may lead to deviation of the eye. Poor vision in an eye because of some other eye disease like cataract, tumours or retinal diseases etc. may also cause the eye to deviate. Therefore it is important in all the cases of squint, especially in children, to have a thorough eye checkup to rule out any other cause of loss of vision.
What are the problems faced by a patient with squint?
When the eyes are not aligned properly, each of the eyes is focusing on a different object and sends different signal to the brain. These two different images reaching the brain lead to various problems that are different in children and adults. In children it can cause suppression of vision in deviating eye causing loss of depth perception (3D vision) and lazy Eye Disease (poor development of vision in the squinting eye) .In adult it may cause confusion or double vision.
What are the symptoms of squint?
in a child, the parents may notice the deviation of eyes. It is important to remember that the eyes of a newborn are rarely aligned at birth. Most establish alignment at 9-10 weeks of age. Therefore squint in any child who is more than two month old must be taken seriously and should be evaluated by an ophthalmologist. Adults may notice double vision, or misalignment of the eyes.
What is the aim of the treatment for squint?
The aims of treatment of squint in order of importance are:
- Preserve or restore vision
- Straighten the eyes for better cosines is
- Restore 3D vision
- Correct any head posture/face turns caused by squint.
When should the squint be treated?
In a child, the treatment of squint and any associated amblyopia should be started as soon as possible. Generally speaking, the younger the age at which amblyopia is treated; the better is the chance of recovery of vision. Remember that the child would never grow out of squint. A delay in treatment may decrease the chances of getting a good alignment and the vision. Earlier the better!
What are the treatment options?
- Glasses
- Patching therapy
- Surgery
Are glasses necessary?
If the child has significant refractive error, glasses are a must. In some cases wearing glasses may correct squint. In other cases, wearing glasses help the eyes to see clearly. This clear vision is very important for the treatment of amblyopia, and also for maintaining the alignment of eyes after they have been aligned by surgery. Remember surgery cannot replace the need for glasses.
Squint surgery
Treatment of squint generally requires eye muscle surgery. However, some patients may need glasses, prisms, medications, or may be best left untreated. The best way to determine whether straightening of the eyes is possible and appropriate, is to undergo an examination by a strabismus surgeon who is experienced in treating squint.
What are the success rates of a squint surgery?
Nearly 80-90% patients are successfully corrected in the straight-ahead position with
one surgery. In some patients the surgery may be only partially successful. In some
patients the eye alignment will change over time, resulting in the need for additional
surgery.
What are the complications of squint surgery?
Squint surgery is an extraocular surgery and hence vision threatening complications are rare.
Like any other surgery, squint surgery is not without complications. Significant complications of strabismus surgery include endophthalmitis (infection of the eye ball) and retinal detachment, both as a result of accidental perforation of the globe during surgery. These complications are very very rare: Perforation of the globe may occur in 0.3% - 2.8% of cases, resulting in endophthalmitis in less than 1:3500 cases, and retinal detachment in even fewer cases.after few months or years. |
| |
|