LASIK is a surgical procedure intended to reduce a person's dependency on glasses or contact lenses. The goal of this Web site is to provide objective information to the public about LASIK surgery. See other sections of this site to learn about what you should know before surgery, what will happen during the surgery, and what you should expect after surgery. There is a glossary of terms and a checklist of issues for you to consider, practices to follow, and questions to ask your doctor before undergoing LASIK surgery.
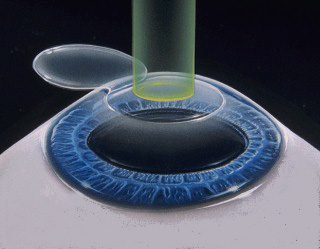
LASIK stands for Laser-Assisted In Situ Keratomileusis and is a procedure that permanently changes the shape of the cornea, the clear covering of the front of the eye, using an excimer laser. A knife, called a microkeratome, is used to cut a flap in the cornea. A hinge is left at one end of this flap. The flap is folded back revealing the stroma, the middlesection of the cornea. Pulses from a computer-controlled laser vaporize a portion of the stroma and the flap is replaced.
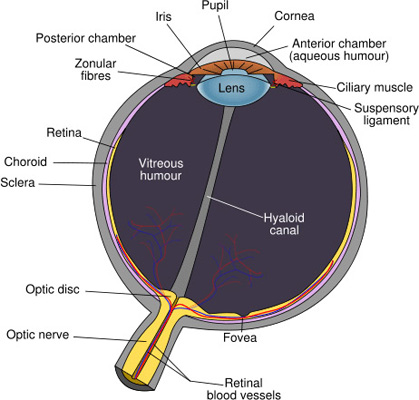
The cornea is a part of the eye that helps focus light to create an image on the retina. It works in much the same way that the lens of a camera focuses light to create an image on film. The bending and focusing of light is also known as refraction. Usually the shape of the cornea and the eye are not perfect and the image on the retina is out-of-focus (blurred) or distorted. These imperfections in the focusing power of the eye are called refractive errors. There are three primary types of refractive errors: myopia, hyperopia and astigmatism. Persons with myopia, or nearsightedness, have more difficulty seeing distant objects as clearly as near objects. Persons with hyperopia, or farsightedness, have more difficulty seeing near objects as clearly as distant objects. Astigmatism is a distortion of the image on the retina caused by irregularities in the cornea or lens of the eye. Combinations of myopia and astigmatism or hyperopia and astigmatism are common. Glasses or contact lenses are designed to compensate for the eye's imperfections. Surgical procedures aimed at improving the focusing power of the eye are called refractive surgery. In LASIK surgery, precise and controlled removal of corneal tissue by a special laser reshapes the cornea changing its focusing power.
Radial Keratotomy or RK and Photorefractive Keratectomy or PRK are other refractive surgeries used to reshape the cornea. In RK, a very sharp knife is used to cut slits in the cornea changing its shape. PRK was the first surgical procedure developed to reshape the cornea, by sculpting, using a laser. Later, LASIK was developed. The same type of laser is used for LASIK and PRK. Often the exact same laser is used for the two types of surgery. The major difference between the two surgeries is the way that the stroma, the middle layer of the cornea, is exposed before it is vaporized with the laser. In PRK, the top layer of the cornea, called the epithelium, is scraped away to expose the stromal layer underneath. In LASIK, a flap is cut in the stromal layer and the flap is folded back.
Another type of refractive surgery is thermokeratoplasty in which heat is used to reshape the cornea. The source of the heat can be a laser, but it is a different kind of laser than is used for LASIK and PRK. Other refractive devices include corneal ring segments that are inserted into the stroma and special contact lenses that temporarily reshape the cornea (orthokeratology).
In the United States, the Food and Drug Administration (FDA) regulates the sale of medical devices such as the lasers used for LASIK. Before a medical device can be legally sold in the U.S., the person or company that wants to sell the device must seek approval from the FDA. To gain approval, they must present evidence that the device is reasonably safe and effective for a particular use, the "indication." Once the FDA has approved a medical device, a doctor may decide to use that device for other indications if the doctor feels it is in the best interest of a patient. The use of an approved device for other than its FDA-approved indication is called "off-label use." The FDA does not regulate the practice of medicine.
-
Regulate a doctor's practice. In other words, FDA does not tell doctors what to do when running their business or what they can or cannot tell their patients.
-
Set the amount a doctor can charge for LASIK eye surgery.
-
"Insist" the patient information booklet from the laser manufacturer be provided to the potential patient.
-
Make recommendations for individual doctors, clinics, or eye centers. FDA does not maintain nor have access to any such list of doctors performing LASIK eye surgery.
-
Conduct or provide a rating system on any medical device it regulates.
The first refractive laser systems approved by FDA were excimer lasers for use in PRK to treat myopia and later to treat astigmatism. However, doctors began using these lasers for LASIK (not just PRK), and to treat other refractive errors (not just myopia). Over the last several years, LASIK has become the main surgery doctors use to treat myopia in the United States. More recently, some laser manufacturers have gained FDA approval for laser systems for LASIK to treat myopia, hyperopia and astigmatism and for PRK to treat hyperopia and astigmatism.
See the section on FDA approved lasers for more details on which lasers have received FDA approval and the specific indications and treatment ranges for which they were approved.
You are probably NOT a good candidate for refractive surgery if:
- You are not a risk taker. Certain complications are unavoidable in a percentage of patients, and there are no long-term data available for current procedures.
- It will jeopardize your career. Some jobs prohibit certain refractive procedures. Be sure to check with your employer/professional society/military service before undergoing any procedure.
- Cost is an issue. Most medical insurance will not pay for refractive surgery. Although the cost is coming down, it is still significant.
- You required a change in your contact lens or glasses prescription in the past year. This is called refractive instability. Patients who are:
- In their early 20s or younger,
- Whose hormones are fluctuating due to disease such as diabetes,
- Who are pregnant or breastfeeding, or
- Who are taking medications that may cause fluctuations in vision, are more likely to have
refractive instability and should discuss the possible additional risks with their doctor.
- You have a disease or are on medications that may affect wound healing. Certain conditions, such as autoimmune diseases (e.g., lupus, rheumatoid arthritis), immunodeficiency states (e.g., HIV) and diabetes, and some medications (e.g., retinoic acid and steroids) may prevent proper healing after a refractive procedure.
- You actively participate in contact sports. You participate in boxing, wrestling, martial arts or other activities in which blows to the face and eyes are a normal occurrence.
- You are not an adult. Currently, no lasers are approved for LASIK on persons under the age of 18.
The safety and effectiveness of refractive procedures has not been determined in patients with some diseases. Do NOT have LASIK surgery if you have a history of any of the following:
-
Herpes simplex or Herpes zoster (shingles) involving the eye area.
-
Glaucoma, glaucoma suspect, or ocular hypertension.
-
Eye diseases, such as uveitis/iritis (inflammations of the eye) and blepharitis (inflammation of the eyelids with crusting of the eyelashes).
-
Eye injuries or previous eye surgeries.
-
Keratoconus
Your doctor should screen you for the following conditions or indicators of risk:
-
Large pupils. Make sure this evaluation is done in a dark room. Younger patients and patients on certain medications may be prone to having large pupils under dim lighting conditions. This can cause symptoms such as glare, halos, starbursts, and ghost images (double vision) after surgery. In some patients these symptoms may be debilitating. For example, a patient may no longer be able to drive a car at night or in certain weather conditions, such as fog.
-
Thin Corneas. The cornea is the thin clear covering of the eye that is over the iris, the colored part of the eye. Most refractive procedures change the eye's focusing power by reshaping the cornea (for example, by removing tissue). Performing a refractive procedure on a cornea that is too thin may result in blinding complications.
-
Previous refractive surgery (e.g., RK, PRK, LASIK). Additional refractive surgery may not be recommended. The decision to have additional refractive surgery must be made in consultation with your doctor after careful consideration of your unique situation.
-
Dry Eyes. LASIK surgery tends to aggravate this condition.
Most patients are very pleased with the results of their refractive surgery. However, like any other medical procedure, there are risks involved. That's why it is important for you to understand the limitations and possible complications of refractive surgery.
Before undergoing a refractive procedure, you should carefully weigh the risks and benefits based on your own personal value system, and try to avoid being influenced by friends that have had the procedure or doctors encouraging you to do so.
- Some patients lose vision. Some patients lose lines of vision on the vision chart that cannot be corrected with glasses, contact lenses, or surgery as a result of treatment.
- Some patients develop debilitating visual symptoms. Some patients develop glare, halos, and/or double vision that can seriously affect nighttime vision. Even with good vision on the vision chart, some patients do not see as well in situations of low contrast, such as at night or in fog, after treatment as compared to before treatment.
- You may be under treated or over treated. Only a certain percent of patients achieve 20/20 vision without glasses or contacts. You may require additional treatment, but additional treatment may not be possible. You may still need glasses or contact lenses after surgery. This may be true even if you only required a very weak prescription before surgery. If you used reading glasses before surgery, you may still need reading glasses after surgery.
- Some patients may develop severe dry eye syndrome. As a result of surgery, your eye may not be able to produce enough tears to keep the eye moist and comfortable. This condition may be permanent. Intensive drop therapy and the use of plugs or other procedures may be required.
- Results are generally not as good in patients with very large refractive errors of any type. You should discuss your expectations with your doctor and realize that you may still require glasses or contacts after the surgery.
- For some farsighted patients, results may diminish with age. If you are farsighted, the level of improved vision you experience after surgery may decrease with age. This can occur if your manifest refraction (a vision exam with lenses before dilating drops) is very different from your cycloplegic refraction (a vision exam with lenses after dilating drops).
- Long-term data is not available. LASIK is a relatively new technology. The first laser was approved for LASIK eye surgery in 1998. Therefore, the long-term safety and effectiveness of LASIK surgery is not known.
Additional Risks if you are Considering the Following:
Monovision is one clinical technique used to deal with the correction of presbyopia, the gradual loss of the ability of the eye to change focus for close-up tasks that progresses with age. The intent of monovision is for the presbyopic patient to use one eye for distance viewing and one eye for near viewing. This practice was first applied to fit contact lens wearers and more recently to LASIK and other refractive surgeries. With contact lenses, a presbyopic patient has one eye fit with a contact lens to correct distance vision, and the other eye fit with a contact lens to correct near vision. In the same way, with LASIK, a presbyopic patient has one eye operated on to correct the distance vision, and the other operated on to correct the near vision. In other words, the goal of the surgery is for one eye to have vision worse than 20/20, the commonly referred to goal for LASIK surgical correction of distance vision. Since one eye is corrected for distance viewing and the other eye is corrected for near viewing, the two eyes no longer work together. This results in poorer quality vision and a decrease in depth perception. These effects of monovision are most noticeable in low lighting conditions and when performing tasks requiring very sharp vision. Therefore, you may need to wear glasses or contact lenses to fully correct both eyes for distance or near when performing visually demanding tasks, such as driving at night, operating dangerous equipment, or performing occupational tasks requiring very sharp close vision (e.g., reading small print for long periods of time).
Many patients cannot get used to having one eye blurred at all times. Therefore, if you are considering monovision with LASIK, make sure you go through a trial period with contact lenses to see if you can tolerate monovision, before having the surgery performed on your eyes. Find out if you pass your state's driver's license requirements with monovision.
In addition, you should consider how much your presbyopia is expected to increase in the future. Ask your doctor when you should expect the results of your monovision surgery to no longer be enough for you to see near-by objects clearly without the aid of glasses or contacts, or when a second surgery might be required to further correct your near vision.
You may choose to have LASIK surgery on both eyes at the same time or to have surgery on one eye at a time. Although the convenience of having surgery on both eyes on the same day is attractive, this practice is riskier than having two separate surgeries.
If you decide to have one eye done at a time, you and your doctor will decide how long to wait before having surgery on the other eye. If both eyes are treated at the same time or before one eye has a chance to fully heal, you and your doctor do not have the advantage of being able to see how the first eye responds to surgery before the second eye is treated.
Another disadvantage to having surgery on both eyes at the same time is that the vision in both eyes may be blurred after surgery until the initial healing process is over, rather than being able to rely on clear vision in at least one eye at all times.
If you are considering refractive surgery, make sure you:
- Compare. The levels of risk and benefit vary slightly not only from procedure to procedure, but from device to device depending on the manufacturer, and from surgeon to surgeon depending on their level of experience with a particular procedure.
- Don't base your decision simply on cost and don't settle for the first eye center, doctor, or procedure you investigate. Remember that the decisions you make about your eyes and refractive surgery will affect you for the rest of your life.
- Be wary of eye centers that advertise, "20/20 vision or your money back" or "package deals." There are never any guarantees in medicine.
- Read. It is important for you to read the patient handbook provided to your doctor by the manufacturer of the device used to perform the refractive procedure. Your doctor should provide you with this handbook and be willing to discuss his/her outcomes (successes as well as complications) compared to the results of studies outlined in the handbook .
Even the best screened patients under the care of most skilled surgeons can experience serious complications.
- During surgery- Malfunction of a device or other error, such as cutting a flap of cornea through and through instead of making a hinge during LASIK surgery, may lead to discontinuation of the procedure or irreversible damage to the eye.
- After surgery. Some complications, such as migration of the flap, inflammation or infection, may require another procedure and/or intensive treatment with drops. Even with aggressive therapy, such complications may lead to temporary loss of vision or even irreversible blindness.
Under the care of an experienced doctor, carefully screened candidates with reasonable expectations and a clear understanding of the risks and alternatives are likely to be happy with the results of their refractive procedure.
If you decide to go ahead with LASIK surgery, you will need an initial or baseline evaluation by your eye doctor to determine if you are a good candidate. This is what you need to know to prepare for the exam and what you should expect:
If you wear contact lenses, it is a good idea to stop wearing them before your baseline evaluation and
switch to wearing your glasses full-time. Contact lenses change the shape of your cornea for up to several weeks after you have stopped using them depending on the type of contact lenses you wear. Not leaving your contact lenses out long enough for your cornea to assume its natural shape before surgery can have negative consequences. These consequences include inaccurate measurements and a poor surgical plan, resulting in poor vision after surgery. These measurements, which determine how much corneal tissue to remove, may need to be repeated at least a week after your initial evaluation and before surgery to make sure they have not changed, especially if you wear RGP or hard lenses. If you wear:
-
soft contact lenses, you should stop wearing them for 2 weeks before your initial evaluation.
-
toric soft lenses or rigid gas permeable (RGP) lenses, you should stop wearing them for at least 3 weeks before your initial evaluation.
-
hard lenses, you should stop wearing them for at least 4 weeks before your initial evaluation.
You should tell your doctor:
- about your past and present medical and eye conditions
- about all the medications you are taking, including over-the-counter medications and any medications you may be allergic to
- whether you are a good candidate
- what the risks, benefits, and alternatives of the surgery are
- what you should expect before, during, and after surgery
- what your responsibilities will be before, during, and after surgery
You should have the opportunity to ask your doctor questions during this discussion. Give yourself plenty of time to think about the risk/benefit discussion, to review any informational literature provided by your doctor, and to have any additional questions answered by your doctor before deciding to go through with surgery and before signing the informed consent form.
You should not feel pressured by your doctor, family, friends, or anyone else to make a decision about having surgery. Carefully consider the pros and cons.
The day before surgery, you should stop using:- creams
- lotions
- makeup
- perfumes
These products as well as debris along the eyelashes may increase the risk of infection during and after surgery. Your doctor may ask you to scrub your eyelashes for a period of time before surgery to get rid of residues and debris along the lashes.
Also before surgery, arrange for transportation to and from your surgery and your first follow-up visit. On the day of surgery, your doctor may give you some medicine to make you relax. Because this medicine impairs your ability to drive and because your vision may be blurry, even if you dont drive make sure someone can bring you home after surgery.
The surgery should take less than 30 minutes. You will lie on your back in a reclining chair in an exam room containing the laser system. The laser system includes a large machine with a microscope attached to it and a computer screen.
A numbing drop will be placed in your eye, the area around your eye will be cleaned, and an instrument called a lid speculum will be used to hold your eyelids open. A ring will be placed on your eye and very high pressures will be applied to create suction to the cornea. Your vision will dim while the suction ring is on and you may feel the pressure and experience some discomfort during this part of the procedure. The microkeratome, a cutting instrument, is attached to the suction ring. Your doctor will use the blade of the microkeratome to cut a flap in your cornea.
The microkeratome and the suction ring are then removed. You will be able to see, but you will experience fluctuating degrees of blurred vision during the rest of the procedure. The doctor will then lift the flap and fold it back on its hinge, and dry the exposed tissue.
The laser will be positioned over your eye and you will be asked to stare at a light. This is not the laser used to remove tissue from the cornea. This light is to help you keep your eye fixed on one spot once the laser comes on. NOTE: if you cannot stare at a fixed object for at least 60 seconds, you may not be a good candidate for this surgery.
When your eye is in the correct position, your doctor will start the laser. At this point in the surgery, you may become aware of new sounds and smells. The pulse of the laser makes a ticking sound. As the laser removes corneal tissue, some people have reported a smell similar to burning hair. A computer controls the amount of laser delivered to your eye. Before the start of surgery, your doctor will have programmed the computer to vaporize a particular amount of tissue based on the measurements taken at your initial evaluation. After the pulses of laser energy vaporize the corneal tissue, the flap is put back into position.
A shield should be placed over your eye at the end of the procedure as protection, since no stitches are used to hold the flap in place. It is important for you to wear this shield to prevent you from rubbing your eye and putting pressure on your eye while you sleep, and to protect your eye from accidentally being hit or poked until the flap has healed.
Immediately after the procedure, your eye may bum, itch, or feel like there is something in it. You may experience some discomfort, or in some cases, mild pain and your doctor may suggest you take a mild pain reliever. Both your eyes may tear.or water. Your vision will probably be hazy or blurry. You will instinctively want to rub your eye, but don't! Rubbing your eye could dislodge the flap, requiring further treatment. In addition, you may experience sensitivity to light, glare, starbursts or haloes around lights, or the whites of your eye may look red or bloodshot. These symptoms should improve considerably within the first few days after surgery. You should plan on taking a few days off from work until these symptoms subside. You should contact your doctor immediately and not wait for your scheduled visit, if you experience severe pain, or if your vision or other symptoms get worse instead of better.
You should see your doctor within the first 24 to 48 hours after surgery and at regular intervals after that for at least the first six months. At the first postoperative visit, your doctor will remove the eye shield, test your vision, and examine your eye. Your doctor may give you one or more types of eye drops to take at home to help prevent infection and/or inflammation. You may also be advised to use artificial tears to help lubricate the eye. Do not resume wearing a contact lens in the operated eye, even if your vision is blurry. You should wait one to three days following surgery before beginning any non-contact sports, depending on the amount of activity required, how you feel, and your doctor's instructions.
To help prevent infection, you may need to wait for up to two weeks after surgery or until your doctor advises you otherwise before using lotions, creams, or make-up around the eye. Your doctor may advise you to continue scrubbing your eyelashes for a period of time after surgery. You should also avoid swimming and using hot tubs or whirlpools for 1-2 months.
Strenuous contact sports such as boxing, football, karate, etc. should not be attempted for at least four weeks after surgery. It is important to protect your eyes from anything that might get in them and from being hit or bumped.
During the first few months after surgery, your vision may fluctuate.
- It may take up to three to six months for your vision to stabilize after surgery.
- Glare, haloes, difficulty driving at night, and other visual symptoms may also persist during this stabilization period. If further correction or enhancement is necessary, you should wait until your eye measurements are consistent for two consecutive visits at least 3 months apart before re-operation.
- It is important to realize that although distance vision may improve after re-operation, it is unlikely that other visual symptoms such as glare or haloes will improve.
- It is also important to note that no laser company has presented enough evidence for the FDA to make conclusions about the safety or effectiveness of enhancement surgery.
Contact your eye doctor immediately, if you develop any new, unusual or worsening symptoms at any point after surgery. Such symptoms could signal a problem that, if not treated early enough, may lead to a loss of vision.
For many people exploring their options in the realm of corrective eye surgery, Monovision might be the answer they've been looking for this whole time.
Monovision is a new LASIK corrective eye surgery procedure, and was approved by the Federal Food and Drug Administration just last year. More formally known as Advanced CustomVue Monovision, the surgery allows the patient to see a particular distance in each eye. In other words, the surgeon corrects the vision so that one eye sees up close, and the other sees far away. It literally takes the prescription of some peoples
glasses, and carves the near prescription to one eye and the far prescription to the other!
As in the case in most LASIK surgeries, patients who have undergone Monovision rarely need glasses again. Furthermore, the patients no longer the minimally magnifying glasses for reading that other with age-related vision deterioration may still need.
This remarkable surgery does take some slight adjusting, but patients who have had the surgery say the slight accommodations they have to make to utilize the right eye at the correct time is minor in comparison to the exponential benefits they've received from better vision.
If you have trouble with your vision for objects both near and far, but have been thus far unable to find a remedy, consult a LASIK surgeon immediately! You could be the next perfect candidate for Monovision LASIK surgery, and the path to better vision is just one consultation away.
For some people exploring LASIK Eye Surgery, news of possible side effects of the surgery causes them enough trepidation to stop the exploration process in it's tracks. Some of the most common side effects of LASIK Surgery are halos and night vision complications. While many people who experience these problems are thrilled they went through with the surgery because of the dramatic improvements to their vision, they still struggle with the effects of halos and night vision complications.
There is, however, good news for people who do experience side effects from LASIK Eye Surgery, as well as people exploring the remarkable procedure but are hesitant about long lasting side effects. Recent studies show that a new eye drop introduced to the shortly after the appearance of halos or night vision complications dramatically reduces common side effects associated with post-laser eye surgery.
The solution that is applied directly to the eye, is known as Brimonidine tartrate, and was tested among subjects in South Korea. The efficacious results of this study have exciting practical implications. For people who are currently living with these annoying side effects, hope is on the horizon. If released widely, this solution promises clearer, more Rerfect vision. For people interested in LASIK surgery, but concerned about the possibilities, Brimonidine tartrate offers a solution to some rare, but known side effects that could spur potential candidates to make a consultation with their nearest LASIK surgeon.
-
-
Ablate in surgery, is to remove.
-
Ablation zone the area of tissue that is removed during laser surgery.
-
Accommodation the ability of the eye to change its focus from distant objects to near objects.
-
Acuity clearness, or sharpness of vision.
-
Astigmatism a distortion of the image on the retina caused by irregularities in the cornea or lens.
-
Bladeless LASIK In the LASIK and Custom LASIK procedures, a flap of corneal tissue must be created and then folded back. With Bladeless LASIK, the surgeon uses the IntraLase laser to create the corneal flap. This technology enables the surgeon the ability to customize the corneal flap for every individual patient.
-
Cornea the clear, front part of the eye. The cornea is the first part of the eye that bends (or refracts) the light and provides most of the focusing power.
-
Diopter the measurement of refractive error. A negative diopter value signifies an eye with myopia and positive diopter value signifies an eye with hyperopia.
-
Dry Eye Syndrome a common condition that occurs when the eyes do not -produce enough tears to keep the eye moist and comfortable. Common symptoms of dry eye include pain, stinging, burning, scratchiness, and intermittent blurring of vision.
-
Endothelium the inner layer of cells on the inside surface of the cornea.
-
Epithelium the outermost layer of cells of the cornea and the eye's first defense against infection.
-
Excimer laser an ultraviolet laser used in refractive surgery to remove corneal tissue.
-
Farsightedness the common term for hyperopia.
-
FDA the abbreviation for the Food and Drug Administration. It is the United States governmental agency responsible for the evaluation and approval of medical devices.
-
Flap & Zap a slang term for LASIK.
-
Ghost Image a fainter second image of the object you are viewing.
-
Glare scatter from bright light that decreases vision.
-
Halos are rings around lights due to optical imperfections in or in front of the eye.
-
Haze corneal clouding that causes the sensation of looking through smoke or fog.
-
Hyperopia the inability to see near objects as clearly as distant objects, and the need for accommodation to see distant objects clearly.
-
Inflammation the body's reaction to trauma, infection, or a foreign substance, often associated with pain, heat, redness, swelling, and/or loss of function.
-
Informed Consent Form a document disclosing the risks, benefits, and alternatives to a procedure.
-
In Situ a Latin term meaning "in place" or not removed.
-
Iris the colored ring of tissue suspended behind the cornea and immediately in front of the lens.
-
Keratectomy the surgical removal of corneal tissue.
-
Keratotomy a surgical incision (cut) of the cornea.
-
Keratitis inflammation of the cornea.
-
Kerato prefix indicating relationship to the cornea.
-
Keratoconus a disorder characterized by an irregular corneal surface (cone-shaped) resulting in blurred and distorted images.
-
Keratomileusis carving of the cornea to reshape it.
-
Laser the acronym for light amplification by stimulated emission of radiation. A laser is an instrument that produces a powerful beam of light that can vaporize tissue.
-
LASIK the acronym for laser assisted in situ keratomileusis which refers to creating a flap in the cornea with a microkeratome and using a laser to reshape the underlying cornea.
-
Lens a part of the eye that provides some focusing power. The lens is able to change shape allowing the eye to focus at different distances.
-
Microkeratome a surgical device that is affixed to the eye by use of a vacuum ring. When secured, a very sharp blade cuts a layer of the cornea at a predetermined depth.
-
Monovision the purposeful adjustment of one eye for near vision and the other eye fordistance vision.
-
Myopia the inability to see distant objects as clearly as near objects.
-
Nearsightedness the common term for myopia.
-
Ophthalmologist a medical doctor specializing in the diagnosis and medical or surgical treatment of visual disorders and eye disease.
-
Optician an expert in the art and science of making and fitting glasses and may also dispense contact lenses.
-
Optometrist a primary eye care provider who diagnoses, manages, and treats disorders of the visual system and eye diseases.
-
Overcorrection a complication of refractive surgery where the achieved amount of correction is more than desired.
-
PRK the acronym for photorefractive keratectomy which is a procedure involving the removal of the surface layer of the cornea (epithelium) by gentle scraping and use of a computer-controlled excimer laser to reshape the stroma.
-
Presbyopia the inability to maintain a clear image (focus) as objects are moved closer. Presbyopia is due to reduced elasticity of the lens with increasing age.
-
Pupil a hole in the center of the iris that changes size in response to changes in lighting. It gets larger in dim lighting conditions and gets smaller in brighter lighting conditions.
-
Radial Keratotomy commonly referred to as RK; a surgical procedure designed to correct myopia (nearsightedness) by flattening the cornea using radial cuts.
-
Refraction a test to determine the refractive power of the eye; also, the bending of light as it passes from one medium into another.
-
Refractive Errors hyperopia, myopia, and astigmatism.
-
Refractive Power the ability of an object, such as the eye, to bend light as light passes through it.
-
Retina a layer of fine sensory tissue that lines the inside wall of the eye. The retina acts like the film in a camera to capture images, transforms the images into electrical signals, and sends the signals to the brain.
-
Sclera the tough, white, outer layer (coat) of the eyeball that, along with the cornea, protects the eyeball.
-
Snellen Visual Acuity Chart one of many charts used to measure vision.
-
Stroma the middle, thickest layer of tissue in the cornea.
-
Undercorrection a complication of refractive surgery where the achieved amount of correction is less than desired.
-
Visual Acuity the clearness of vision; the ability to distinguish details and shapes.
-
Vitreous Humor the transparent, colorless mass of gel that lies behind the lens and in front of the retina and fills the center of the eyeball.
With so many people opting to correct their less than perfect vision with a laser procedure, how can you truly know which procedure you read about is right for you? There is a lot of confusion among consumers about PRK, RK, LASIK, and Custom LASIK. While only your carefully selected eye surgeon will know for sure which procedure is right for you, you can have an idea of what is involved with what before even going into the consultation.
RK is formally known as Radial Ker.atotomy, and is the original procedure that spurred the technology of the later ones. The cornea is flattened out by using a scalpel to make an incision. Most surgeons now opt for a higher technology procedure, but you may still be able to locate surgeons who will do this procedure.
PRK stands for photorefractive keratectomy, and involves the use of the laser in the process of the cornea reshaping. The outside layer is scraped away in PRK, allowing the surgeon access to the cornea. Again, most laser eye surgeons have opted instead for the now FDA-approved LASIK surgery to the relatively "ancient" RK and PRK. However, PRK s still being performed on certain patients who are not considered candidates for LASIK, but are qualified for PRK.
LASIK is now the mainstream laser surgery that most people know and millions of Americans have successfully undergone with unbelievable results. Instead of scraping the outer layer of the cornea away, doctors use a tiny blade to make a flap in the cornea. The cornea is shaped with the laser, and the flap is put back into place.
Finally, the most state-of-the-art laser surgery available now is Custom LASIK. The primary difference between this and conventional LASIK is this: instead of gaining access to the inner parts of the cornea by using a blade, another laser is used, negating the use of any blade near any part of the eye, and drastically reducing the chances of human error. Whatever procedure sounds best for you, you must schedule a consultation with a nearby LASIK surgeon.
Lasik Eye Surgery is one of the most common elective surgical procedures in the world, with over 1 million Americans undergoing the vision correction treatment every year. LASIK is commonly used for patients with myopia and hyperopia, but can possibly be used on other vision problems. It is an outpatient procedure that takes only a few minutes for the actual procedure from beginning to end, and is virtually painless with few side effects.
The success rate of this surgery is perhaps the most appealing aspect of it, and the reason why it is so popular. Because patients suffering from nearsightedness, farsightedness, astigmatism and prebyopia are all good candidates for LASIK Eye Surgery, many people dealing with a variety of vision problems are able to get results from this surgery.
LASIK Surgery is not performed on children under 18, pregnant women, and certain vision conditions that would disqualify you from the surgery. If you're interested in LASIK Eye Surgery, schedule a consultation with a LASIK surgeon. He or she will be able to tell you if you're a good candidate for the surgery, and if so, you can join the ranks of the millions of people who were able to throw away their glasses!
Who has more riding on their eyes than scores of professional athletes that make millions of dollars for the talent and skill associated with their eyes. These athletes depends on their eyes for their lucrative livelihood, fame, and popularity, and stand to lose more than just millions of dollars should something go wrong.
Yet, every year, hundreds of professional athletes, as well as government aviators, CEOs, actors, models and (gasp!) DOCTORS undergo LASIK Eye Surgery every year. Why would they take such a risk when they stand to lose so much? Because LASIK Surgery is one of the most successful procedures, elective or otherwise that someone can have! LASIK takes only minutes, is relatively painless, and allows the patient to be back doing everyday things, such as working and driving, by the next day. Moreover, new technology has eliminated the need for a blade at all. This new procedure, known as IntraLASIK uses a laser to make reach the inner layers of the cornea. No longer is there a risk of a slip or complication while the surgeon holds a knife. IntraLASIK has recently been approved by the United States Government to be performed on some of their most treasured personnel - an approval that they did not give before.
So, on the replays, when you see Tiger Woods look so intently at that 19th hole at the U.S. Open, know that he is looking with vision far superior than he ever had before. He stood to lose lots, but because of the remarkably low risk, he ended up winning big.
The slowing economy is responsibly for a lot of trends we haven't been seeing in the past several years. Higher food prices, higher energy costs, a slumping real estate. But perhaps the most telling trend is the decline of elective surgical procedures. After all, in our image-obsessed society, we tread through a mass of plastic surgery reality shows that make us all believe the perfect body/nose/chest/face is a mere 30 minutes away.
Because of the societal change in attitude about cosmetic surgery, it was especially alarming that so many cosmetic surgeries were on the decline. Eyelid surgeries are down about 30%, and facial contouring is down 40%. Even everyday options like dental procedures, such as orthodontia and implants are on the decline.
Experts say anything that is not covered by health insurance is eligible for being on the fritz.
So what does this mean for the millions of people who were hoping to finally get the LASIK surgery they've dreamed of for years, but is not being covered by their health insurance? Well, the interpretation is quite good! Because LASIK surgeons are allowed to compete in a free market system (meaning, they're allowed to advertise and competitively price their services), some of the best LASIK centers and surgeons in the entire world are dropping their prices to re-attract the masses that were once flocking in a booming economy. This means prices for you are about 50% lower than they were two years ago.
If you want to get LASIK eye surgery, book your free consultation now. There is no time like the present to
reap the benefits of a slumping economy. And the longer you wait and toil over this decision, the higher the
prices are going to slowly climb.