|
|
|||||||||||
| HOME | I |
ABOUT DR. | I | TREATMENT | I | GALLERY | I | CHAMBERS | I | SURGICAL VIDEOS | I | FAQ | I | CONTACT |





| HIGH RISK PREGNANCY : | |||
|---|---|---|---|
A high-risk pregnancy is one that threatens the health or life of the mother or her fetus. For most women, early and regular prenatal care promotes a healthy pregnancy and delivery without complications. But some women are at an increased risk for complications even before they get pregnant for a variety of reasons.Risk factors for a high-risk pregnancy can include: |
|||
|
 |
||
| Women with high-risk pregnancies should receive care from a special team of health care providers to ensure that their pregnancies are healthy and that they can carry their infant or infants to term. | |||
| What are the factors that put a pregnancy at risk ? | |||
| The factors that place a pregnancy at risk can be divided into four categories : | |||
|
|||
| Existing Health Conditions | |||
|
 |
||
|
|||
|
 |
||
| Age | |||
|
|||
|
|||
| Lifestyle Factors | |||
|
 |
||
Conditions of Pregnancy |
|||
|
 |
||
|
|||
| PREGNANCY COUNSELING: | |||
The PC Program provides counseling to women who need assistance with decision-making and the emotional stress of an unplanned pregnancy. The infant’s needs are also of utmost importance. We also provide services to the baby’s father and the parents’ families, when appropriate and when not in conflict with the client’s wishes. Pregnancy Counseling services are available to expectant or newly parenting single or married women. Most clients are single women between 15 and 25 who have never before given birth and who contact the agency in the early to middle of their pregnancy. However, some are older or younger, some are married, divorced or separated. Some have other children. Some contact the agency after delivery. Occasionally a client will bring her baby home for a period of time, then seek counseling about adoption when she feels she cannot parent adequately. |
 |
||
The goal of the PC Program is to assist the client in making a comfortable informed plan for herself and her baby. We provide accurate objective information about all their options and encourage her to make an informed independent decision. We offer her an opportunity to explore all her options in the context of her own life, her goals, relationships, values and available resources. Prevention of future pregnancies is also explored and clients are encouraged to consult with their doctor about their family planning options. |
|||
Services include immediate, objective, in-depth counseling beyond the “options counseling” offered in other programs. We do not impose a set of values or religious tenets upon our clients and our counseling is provided by a master’s level clinical staff. The program is community based and we work with other providers involved.
|
 |
||
Services are available in New Hampshire, south of Lebanon, and in bordering states if the client delivers in New Hampshire and the travel distance is manageable. |
|||
| INFERTILITY SOLUTION : | |||
What is male infertility?
Reproduction (or making a baby) is a simple and natural experience for most couples. However, for some couples it is very difficult to conceive. A man’s fertility generally relies on the quantity and quality of his sperm. If the number of sperm a man ejaculates is low or if the sperm are of a poor quality, it will be difficult, and sometimes impossible, for him to cause a pregnancy. Male infertility is diagnosed when, after testing both partners, reproductive problems have been found in the male. How common is male infertility? |
 |
||
Infertility is a widespread problem. For about one in five infertile couples the problem lies solely in the male partner. It is estimated that one in 20 men has some kind of fertility problem with low numbers of sperm in his ejaculate. However, only about one in every 100 men has no sperm in his ejaculate. |
|||
|
|||
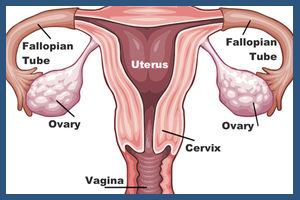
| What causes female infertility?
|
|
||
| The most common causes of female infertility include problems with ovulation, damage to fallopian tubes or uterus, or problems with the cervix. Age can contribute to infertility because as a woman ages, her fertility naturally tends to decrease.
|
|||
Damage to the fallopian tubes or uterus can be caused by one or more of the following:
|
|||
 Abnormal cervical mucus can also cause infertility. Abnormal cervical mucus can prevent the sperm from reaching the egg or make it more difficult for the sperm to penetrate the egg. Abnormal cervical mucus can also cause infertility. Abnormal cervical mucus can prevent the sperm from reaching the egg or make it more difficult for the sperm to penetrate the egg.How is female infertility diagnosed? Potential female infertility is assessed as part of a thorough physical exam. The exam will include a medical history regarding potential factors that could contribute to infertility. Healthcare providers may use one or more of the following tests/exams to evaluate fertility:
|
|||
| How is female infertility treated? |  |
||
Female infertility is most often treated by one or more of the following methods:
|
|||
| Can female infertility be prevented?
|
|||
T here is usually nothing that can be done to prevent female infertility caused by genetic problems or illness. here is usually nothing that can be done to prevent female infertility caused by genetic problems or illness.
|
|||
| OVARIAN CYST | |||
| What is a cyst? | |||
| A cyst is a closed sac-like structure - an abnormal pocket of fluid, similar to a blister - that contains either liquid, gaseous, or semi-solid material. A cyst is located within the tissue, and can develop anywhere in the body and may vary in size - some are so tiny they can only be observed through a microscope, while others may become so large that they displace normal organs. In anatomy, a cyst can also refer to any normal bag or sac in the body, such as the bladder. In this text, cyst refers to an abnormal sac or pocket in the body that contains either liquid, gaseous or semi-solid substances. |
 |
||
| A cyst is not a normal part of the tissue where it is located. It has a distinct membrane and division on nearby tissue - the outer or capsular portion of a cyst is called the cyst wall. If the sac is filled with pus it is not a cyst, it is an abscess. Some cysts are solid and may be called tumors (pathological cysts). The word tumor does not necessarily mean it is cancerous - a tumor is a medical term for a swelling. |
|||
| Causes of ovarian cysts | |||
 In this section we look at the causes of ovarian cysts. As the causes are different for each type of ovarian cyst, we will look at each type one at a time. In this section we look at the causes of ovarian cysts. As the causes are different for each type of ovarian cyst, we will look at each type one at a time.Functional ovarian cysts
There are two types of functional ovarian cysts: 1) Follicular cysts Follicular cysts are the most common type of ovarian cyst. A female human has two ovaries, small round organs which release an egg every month. The egg moves into the uterus (womb), where it can be fertilized by a male sperm. The egg is formed in the follicle, which contains fluid to protect the growing egg. When the egg is released, the follicle bursts. In some cases, the follicle either does not shed its fluid and shrink after releasing the egg, or does not release an egg. The follicle swells with fluid, becoming a follicular ovarian cyst. Typically, one cyst appears at any one time and normally goes away within a few weeks (without treatment).
Pathological cysts Dermoid cysts are the most common type of pathological cyst for women under 30 years of age. Cystadenomas are more common among women aged over 40 years. Dermoid cysts (cystic teratomas) A dermoid cyst a bizarre tumor, usually benign. This type of cyst develops from a totipotential germ cell (a primary oocyte) - in other words, the cell can give rise to all orders of cells necessary to form mature tissues. Dermoid cysts contain hair, skin, bone and other tissues (sometimes even teeth). A totipotential germ cell can develop in any direction. They are formed from cells that make eggs. These cysts need to be removed surgically. Cystadenomas Cystadenomas are ovarian cysts that develop from cells that cover the outer part of the ovary. Some are filled with a thick, mucous substance, while others contain a watery liquid. Rather than growing inside the ovary itself, cystadenomas are usually attached to the ovary by a stalk. By existing outside the ovary, they have the potential to grow considerably. Although they are rarely cancerous, they need to be removed surgically. Endometriosis Endometriosis is a condition in which cells that are normally found inside the uterus (endometrial cells) are found growing outside of the uterus. That is the lining of the inside of the uterus is found outside of it. Endometrial cells are the cells that shed every month during menstruation, and so endometriosis is most likely to affect women during their childbearing years. Women with this condition have a higher risk of developing ovarian cysts. Polycystic ovarian syndrome (PCOS) In this condition many small and harmless cysts develop on the ovaries, caused by a problem with hormone balance produced by the ovaries. People with PCOS have a higher risk of developing ovarian cysts. |
|||
Symptoms of ovarian cysts |
|||
| A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor detect. For example, pain may be a symptom while a rash may be a sign. In the vast majority of cases, ovarian cysts are small and benign (harmless); there will be no signs or symptoms. Even if there are symptoms, they alone cannot determine whether a patient has an ovarian cyst. There are several other conditions with similar signs and symptoms, including endometriosis, pelvic inflammatory disease, ectopic pregnancy or ovarian cancer. A ruptured ovarian cyst may present similar signs and symptoms to those of appendicitis or diverticulitis. |
|||
| Signs and symptoms of an ovarian cyst may include: | |||
|
|||
| HYSTERECTOMY | |||
| What Is a Hysterectomy? A hysterectomy is a surgical procedure to remove a woman’s uterus. The uterus, also known as the womb, is where a baby grows when a woman is pregnant. The uterine lining is the source of menstrual blood. You may need a hysterectomy for many reasons. The surgery can be used to treat a number of chronic pain conditions as well as certain types of cancer and infections. |
|||
Why Is a Hysterectomy Performed? Your doctor may suggest a hysterectomy if you have any of the following: |
|||
|
|||
| What Are the Types of Hysterectomy? There are several different types of hysterectomy. During a partial hysterectomy, your doctor removes only a portion of your uterus. They may leave your cervix intact. Hysterectomy and Salpingo-Oophorectomy During a hysterectomy and salpingo-oophorectomy, your doctor removes the uterus along with one or both of your ovaries and fallopian tubes. You may need hormone replacement therapy if both of your ovaries are removed. How Is a Hysterectomy Performed? A hysterectomy can be performed in several ways. All methods require a general or local anesthetic. A general anesthetic will put you to sleep throughout the procedure so that you don’t feel any pain. A local anesthetic will numb your body below the waistline, but you’ll remain awake during the surgery. This type of anesthetic will sometimes be combined with a sedative, which will help you feel sleepy and relaxed during the procedure. Abdominal Hysterectomy During an abdominal hysterectomy, your doctor removes your uterus through a large cut in your abdomen. The incision may be vertical or horizontal. Both types of incisions tend to heal well and leave little scaring. Vaginal Hysterectomy During a vaginal hysterectomy, your uterus is removed through a small incision made inside the vagina. There are no external cuts, so there won’t be any visible scars. Laparoscopic Hysterectomy During a laparoscopic hysterectomy, your doctor uses a tiny instrument called a laparoscope. A laparoscope is a long, thin tube with a high-intensity light and a high-resolution camera at the front. The instrument is inserted through incisions in the abdomen. Three or four small incisions are made instead of one large incision. Once the surgeon can see your uterus, they’ll cut the uterus into small pieces and remove one piece at a time. What Are the Risks of a Hysterectomy? A hysterectomy is considered to be a fairly safe procedure. As with all major surgeries, however, there are associated risks. Some people may have an adverse reaction to the anesthetic. There is also the risk of heavy bleeding and infection around the incision site. |
|||
|
|||
| These risks are rare. However, if they occur, you may need a second surgery to correct them. | |||
| Recovering from a Hysterectomy After your hysterectomy, you’ll need to spend two to five days in the hospital. Your doctor will give you medication for the pain and monitor your vital signs, such as your breathing and heart rate. You’ll also be encouraged to walk around the hospital as soon as possible. Walking helps prevent blood clots from forming in the legs. If you’ve had a vaginal hysterectomy, your vagina will be packed with gauze to control the bleeding. The doctors will remove the gauze within a few days after the surgery. However, you may experience bloody or brownish drainage from your vagina for about 10 days. Wearing a menstrual pad can help protect your clothing from getting stained. When you return home from the hospital, it’s important to continue walking. You can walk around inside your house or around your neighborhood. However, you should avoid performing certain activities during recovery. These include:
|
|||
|
|||
If you’ve had a vaginal or laparoscopic hysterectomy, you’ll probably be able to return to most of your regular activities within three to four weeks. Recovery time will be a little longer if you’ve had an abdominal hysterectomy. You should be completely healed in about four to six weeks. |
|||
| UTERINE FIBROIDS | |||
Uterine fibroids are very common non-cancerous (benign) growths that develop in the muscular wall of the uterus. They can range in size from very tiny (a quarter of an inch) to larger than a cantaloupe. Occasionally, they can cause the uterus to grow to the size of a five-month pregnancy. In most cases, there is more than one fibroid in the uterus. While fibroids do not always cause symptoms, their size and location can lead to problems for some women, including pain and heavy bleeding. Fibroids can dramatically increase in size during pregnancy. This is thought to occur because of the increase in estrogen levels during pregnancy. After pregnancy, the fibroids usually shrink back to their pre-pregnancy size. They typically improve after menopause when the level of estrogen, the female hormone that circulates in the blood, decreases dramatically. However, menopausal women who are taking supplemental estrogen (hormone replacement therapy) may not experience relief of symptoms. |
|||
| Uterine Fibroid Symptoms | |||
| Most fibroids don’t cause symptoms—only 10 to 20 percent of women who have fibroids require treatment. Depending on size, location and number of fibroids, they may cause: | |||
|
|||
| Uterine Fibroid Treatments | |||
| Watchful waiting Many women with uterine fibroids experience no signs or symptoms, or only mildly annoying signs and symptoms that they can live with. If that's the case for you, watchful waiting could be the best option. Fibroids aren't cancerous. They rarely interfere with pregnancy. They usually grow slowly — or not at all — and tend to shrink after menopause, when levels of reproductive hormones drop. |
|||
| Medications Medications for uterine fibroids target hormones that regulate your menstrual cycle, treating symptoms such as heavy menstrual bleeding and pelvic pressure. They don't eliminate fibroids, but may shrink them. Medications include: |
|||
Many women have significant hot flashes while using Gn-RH agonists. Gn-RH agonists typically are used for no more than three to six months because symptoms return when the medication is stopped and long-term use can cause loss of bone.
|
|||
| Nonsteroidal anti-inflammatory drugs (NSAIDs), which are not hormonal medications, may be effective in relieving pain related to fibroids, but they don't reduce bleeding caused by fibroids. Your doctor may also suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia. | |||
|
||||||||
| HOME I ABOUT DR. I TREATMENT I GALLERY I CHAMBERS I SURGICAL VIDEOS I FAQ I CONTACT | ||||||||
TREATMENT |
||||||||
| HIGH RISK PREGNANCY I PREGNANCY COUNSELING I INFERTILITY SOLUTION I OVARIAN CYST I HYSTERECTOMY I UTERINE FIBROIDS | ||||||||
Site Powered By : www.calcuttayellowpages.com |
||||||||
 What are the symptoms of male infertility?
What are the symptoms of male infertility? About two-thirds of infertile men have a problem with making sperm in the testes. Either low numbers of sperm are made and/or the sperm that are made do not work properly.
About two-thirds of infertile men have a problem with making sperm in the testes. Either low numbers of sperm are made and/or the sperm that are made do not work properly. 

 Pelvic exam and breast exam
Pelvic exam and breast exam